The symptoms of sciatica may range from infrequent and irritating to severe and debilitating. Sciatica symptoms depend on the specific spinal nerve root that is irritated and/or compressed in the lower spine. One or more nerve roots may be affected together.
While some symptoms are specific to nerve roots, other symptoms are common and occur in all sciatica types.
Common Sciatica Symptoms
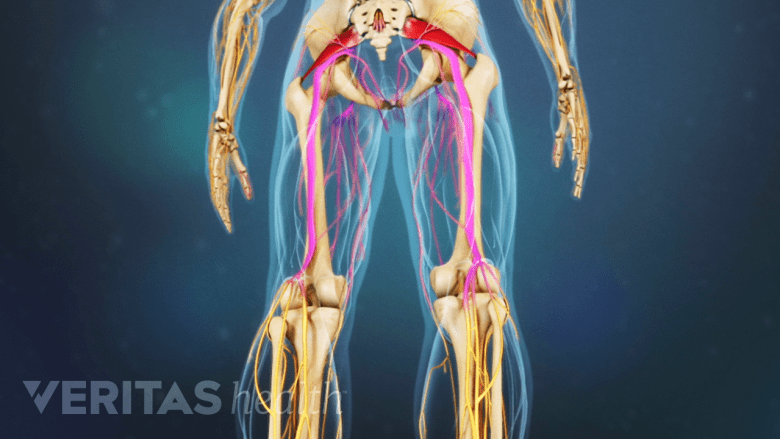
Usually, sciatica affects only one leg at a time and the symptoms radiate from the lower back or buttock to the thigh and down the leg. Sciatica may cause pain in the front, back, and/or sides of the thigh and leg.
A few common symptoms seen in sciatica are:
- Pain. Sciatica pain may be constant or intermittent. The pain is usually described as a burning sensation or a sharp, shooting pain. The pain is usually more severe in the leg compared to the back. Leg pain commonly occurs more in the calf region below the knee compared to other parts of the leg.
- Altered sensation. Numbness, tingling, and/or a pins-and-needles sensation may be felt at the back of the leg.
- Weakness. Weakness may be felt in the leg and foot. A feeling of heaviness in the affected leg may make it difficult to lift the foot off the floor.
- Change in posture may aggravate or relieve pain. Certain postures may affect sciatica pain:
- Sciatica pain may feel worse while sitting, trying to stand up, standing for a long time, bending the spine forward, twisting the spine, and/or while coughing.
Pain may increase or remain constant while lying down, causing disturbed sleep.1Kumar, M. Epidemiology, pathophysiology and symptomatic treatment of sciatica: A review. nt. J. Pharm. Bio. Arch. 2011, 2. Lying on the back with the knees slightly elevated and propped up with a pillow, or lying on the side with a pillow between the legs, may help relieve the pain in such cases.
The pain may be relieved while walking, applying a heat pack to the rear pelvic area, or doing pelvic exercises.
There may be other sciatica symptoms that are specific to the affected nerve root. The sciatic nerve is formed by the combination of 5 nerve roots: L4, L5, S1, S2, and S3.
In This Article:
Sciatica Symptoms for Each Nerve Root

Each nerve root produces a set of unique sciatica symptoms.
Sciatica symptoms typically occur when L4, L5, and/or S1 nerve roots are affected.2Hernández C.P., Sanchez N., Navarro-Siguero A., Saldaña M.T. (2013) What is Sciatica and Radicular Pain?. In: Laroche F., Perrot S. (eds) Managing Sciatica and Radicular Pain in Primary Care Practice. Springer Healthcare, Tarporley. https://doi.org/10.1007/978-1-907673-56-6_1 Sciatica symptoms arising from each of these nerve roots are discussed below3Ngnitewe Massa R, Mesfin FB. Herniation, Disc. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/,4Wright R, Inbody SB. Radiculopathy and Degenerative Spine Disease. In: Neurology Secrets. Elsevier; 2010:121-130. doi:10.1016/b978-0-323-05712-7.00007-6:
- Sciatica from the L4 nerve root may cause:
- Pain, in the hip, thigh, and the inner (medial) areas of the knee and calf.
- Loss of sensation over the inner calf.
- Weakness in the thigh muscles and the hip muscles that help pull the legs together.
- Loss of tendon reflex in the knee (reduced knee-jerk reflex).
- Sciatica from the L5 nerve root may cause:
- Pain in the buttock and the outer (lateral) part of the thigh and leg.
- Loss of sensation in the area of skin in between and over the great toe and the second toe.
- Weakness in the buttock and leg muscles.
- Difficulty in moving the ankle and in lifting the great toe upward.
- Sciatica from the S1 nerve root, also called classic sciatica, may cause:
- Pain in the buttock, back of the calf, and side of the foot.
- Loss of sensation in the outer side of the foot, including the third, fourth, and fifth toes.
- Difficulty while raising the heel off the ground or walking on tiptoes.
- Weakness in the buttock and foot muscles.
- Loss of tendon reflex in the ankle (reduced ankle-jerk reflex).
Sciatica pain mostly occurs when the nerve roots are irritated due to an inflammatory condition such as a herniated disc or pelvic muscle spasm. If a nerve is compressed, the symptoms are usually severe, resulting in marked weakness and loss of function in the leg.5Davis D, Vasudevan A. Sciatica. [Updated 2019 Feb 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/
See Understanding Sciatica Symptoms: Pins and Needles, Numbness, Icy, and Burning
Types of Sciatica
Bilateral sciatica affects both legs at the same time.
Depending on the duration of symptoms and if one or both legs are affected, sciatica can be of different types:
- Acute sciatica. Acute sciatica is a recent onset, 4 to 8-week duration of sciatic nerve pain. The pain may be self-managed and may not typically require medical treatment.1Kumar, M. Epidemiology, pathophysiology and symptomatic treatment of sciatica: A review. nt. J. Pharm. Bio. Arch. 2011, 2.
- Chronic sciatica. Chronic sciatica is persistent sciatic nerve pain that lasts for more than 8 weeks and usually does not subside with self-management. Depending on the cause, chronic sciatica may require nonsurgical or surgical treatment.1Kumar, M. Epidemiology, pathophysiology and symptomatic treatment of sciatica: A review. nt. J. Pharm. Bio. Arch. 2011, 2.
- Alternating sciatica. Alternating sciatica is sciatic nerve pain that affects both legs alternately. This type of sciatica is rare and may result from degenerative problems in the sacroiliac joint.6Ombregt L. The dural concept. In: A System of Orthopaedic Medicine. Elsevier; 2013:447-472.e4. doi:10.1016/b978-0-7020-3145-8.00033-8
- Bilateral sciatica. Bilateral sciatica occurs in both legs together. This type of sciatica is rare and may occur due to degenerative changes in the vertebrae and/or the disc at several spinal levels, or from serious conditions such as cauda equina syndrome.6Ombregt L. The dural concept. In: A System of Orthopaedic Medicine. Elsevier; 2013:447-472.e4. doi:10.1016/b978-0-7020-3145-8.00033-8
Read more about Types of Sciatic Nerve Pain
Informally, the term wallet sciatica may be used to describe sciatic pain that occurs while sitting on a wallet (or any object in the back pocket of a trouser).
The treatment of sciatica is focused on addressing the cause of symptoms. It’s important to consult with a doctor for a correct diagnosis, to check for the possibility of a serious medical problem, and for effective treatment.
- 1 Kumar, M. Epidemiology, pathophysiology and symptomatic treatment of sciatica: A review. nt. J. Pharm. Bio. Arch. 2011, 2.
- 2 Hernández C.P., Sanchez N., Navarro-Siguero A., Saldaña M.T. (2013) What is Sciatica and Radicular Pain?. In: Laroche F., Perrot S. (eds) Managing Sciatica and Radicular Pain in Primary Care Practice. Springer Healthcare, Tarporley. https://doi.org/10.1007/978-1-907673-56-6_1
- 3 Ngnitewe Massa R, Mesfin FB. Herniation, Disc. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/
- 4 Wright R, Inbody SB. Radiculopathy and Degenerative Spine Disease. In: Neurology Secrets. Elsevier; 2010:121-130. doi:10.1016/b978-0-323-05712-7.00007-6
- 5 Davis D, Vasudevan A. Sciatica. [Updated 2019 Feb 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/
- 6 Ombregt L. The dural concept. In: A System of Orthopaedic Medicine. Elsevier; 2013:447-472.e4. doi:10.1016/b978-0-7020-3145-8.00033-8

