Sacroiliac (SI) joint injections are effective in diagnosing and managing lower back pain; however, like any medical procedure, SI joint injections are not without potential side effects and risks. Understanding the risks and potential outcomes is crucial in making an informed decision about undergoing this type of procedure.
Patients are advised to discuss the risks, benefits, and alternatives to injection treatments with the treating physician before consenting to the procedure.
In This Article:
- Sacroiliac Joint Injection for Lower Back Pain
- Sacroiliac Joint Injection: Procedure, Pain Relief, and Recovery
- Sacroiliac Joint Injections: Risks, Success Rates, and Long-Term Outcomes
- Sacroiliac Joint Steroid Injection Video
Potential Side Effects of SI Joint Steroid Injections

A temporary increase in pain may be experienced after the injection.
As with any injection procedure, SI joint injections may cause side effects. These are usually minor and temporary.
Common side effects of SI joint injections include:
- Pain at the injection site. The pain is typically due to the needle insertion and the initial irritation from the medication and is the most common side effect.1Foster ZJ, Voss TT, Hatch J, Frimodig A. Corticosteroid Injection for Common Musculoskeletal Conditions. Am Fam Physician. 2015;92(8):694-699. https://pubmed.ncbi.nlm.nih.gov/26554409/
- Leg numbness or weakness. The local anesthetic used in the injection can cause temporary numbness or weakness in the legs. This side effect usually wears off within a few hours after the procedure.1Foster ZJ, Voss TT, Hatch J, Frimodig A. Corticosteroid Injection for Common Musculoskeletal Conditions. Am Fam Physician. 2015;92(8):694-699. https://pubmed.ncbi.nlm.nih.gov/26554409/
- Increased lower back pain. Some patients may experience a temporary increase in their usual pain following the injection. This symptom is often due to the irritation of the surrounding structures caused by the needle. This pain usually resolves within a few days.2Cohen SP, Chen Y, Neufeld NJ. Sacroiliac Joint Pain: A Comprehensive Review of Epidemiology, Diagnosis and Treatment. Expert Rev Neurother. 2013;13(1):99-116. http://doi.org/10.1586/ern.12.148
It’s important to note that while these side effects are possible, they are not guaranteed to occur. Many patients undergo SI joint injections without experiencing any side effects.1Foster ZJ, Voss TT, Hatch J, Frimodig A. Corticosteroid Injection for Common Musculoskeletal Conditions. Am Fam Physician. 2015;92(8):694-699. https://pubmed.ncbi.nlm.nih.gov/26554409/ However, if pain and weakness do not subside within a few days, it’s important to contact your physician.
Potential Risks of SI Joint Steroid Injections
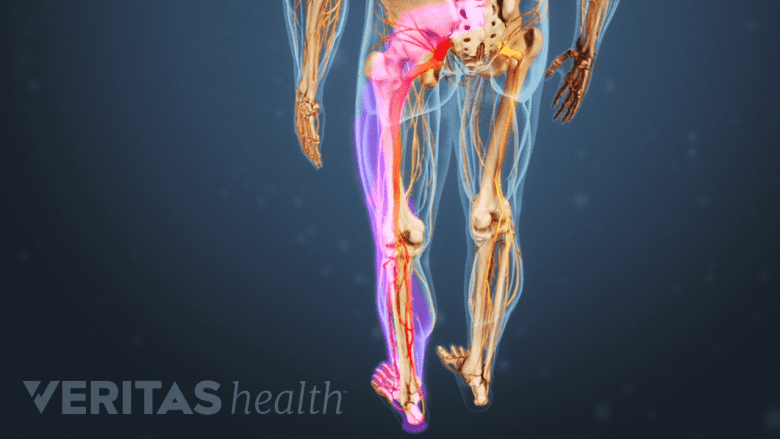
Nerve damage due to the injection may lead to numbness and tingling in the leg.
While serious complications are rare, they can occur.
Potential risks and adverse events of SI joint injections include:
- Nerve damage. There is a possibility of unintentional nerve injury by the needle during the procedure, which can cause numbness, tingling, or weakness in the leg.
This risk is minimized by using fluoroscopy or ultrasound to help visualize anatomical structures. - Infection. While rare, any procedure that involves breaking the skin risks infection. Infections may require treatment with antibiotics or, in severe cases, surgery.
This risk is minimized by proper cleaning of the injection site before needle insertion. - Adverse reaction to the injectate. Some people may have an adverse reaction to the medication used in the injection. Adverse reactions include allergic reactions or side effects from the medication.
- Bleeding or bruising at the injection site. While rare, the risk of bleeding or bruising is most common in people with a bleeding disorder or who are taking blood thinners.1Foster ZJ, Voss TT, Hatch J, Frimodig A. Corticosteroid Injection for Common Musculoskeletal Conditions. Am Fam Physician. 2015;92(8):694-699. https://pubmed.ncbi.nlm.nih.gov/26554409/
The probability of these complications is relatively low, and when indicated, the procedure’s benefits typically outweigh the risks when treating lower back pain.1Foster ZJ, Voss TT, Hatch J, Frimodig A. Corticosteroid Injection for Common Musculoskeletal Conditions. Am Fam Physician. 2015;92(8):694-699. https://pubmed.ncbi.nlm.nih.gov/26554409/
Success Rates of SI Joint Steroid Injections

The majority of individuals experience relief following an SI joint injection.
Studies have shown that SI joint injections may provide significant pain relief for at least 1 month in the majority of patients with SI joint pain. For example, a small study involving 10 participants who received SI joint injections for SI joint pain showed that 80% of people experienced a 90% reduction in pain relief that lasted for 3 months.3Klauser A, Zordo TD, Feuchtner G, Sogner P, Schirmer M, Gruber J, Sepp N, Moriggl B. Feasibility of Ultrasound-Guided Sacroiliac Joint Injection Considering Sonoanatomic Landmarks at Two Different Levels in Cadavers and Patients. Arthritis & Rheumatism (Arthritis Care & Research). 2009, 59(11):1618-1624. http://doi.org/10.1002/art.24204
The success of the procedure depends on the accurate identification of the SI joint as the primary cause of the patient’s pain, as well as the duration of symptoms, severity of pain, and the patient’s overall health.
Number of SI Joint Injections Needed for Complete Pain Relief

The number of SI joint injections necessary for effective pain relief can vary between individuals.
The goal of SI joint injections is to provide enough pain relief to allow the patient to improve their functional status. Participation in physical therapy or exercise is encouraged, which can lead to longer-term improvements in pain and function. The number of SI joint injections required for effective pain relief can vary depending on the patient.
Some patients may only require one injection, while others may require several injections. As a general guideline, injections may be administered once every 2 weeks, and no more than 3 injections may be given per year.2Cohen SP, Chen Y, Neufeld NJ. Sacroiliac Joint Pain: A Comprehensive Review of Epidemiology, Diagnosis and Treatment. Expert Rev Neurother. 2013;13(1):99-116. http://doi.org/10.1586/ern.12.148,4D'Orazio F, Gregori LM, Gallucci M. Spine epidural and sacroiliac joints injections - when and how to perform. Eur J Radiol. 2015;84(5):777-782. http://doi:10.1016/j.ejrad.2014.05.039
In general, if the first injection provides significant relief, additional injections may be recommended. However, the exact timing can vary based on the doctor’s guidance, the patient’s response to the treatment, and the type of injection.1Foster ZJ, Voss TT, Hatch J, Frimodig A. Corticosteroid Injection for Common Musculoskeletal Conditions. Am Fam Physician. 2015;92(8):694-699. https://pubmed.ncbi.nlm.nih.gov/26554409/
Long-Term Outcomes of SI Joint Injections
The long-term outcomes of SI joint injections can vary depending on a number of factors, including the underlying cause of the pain, the patient’s overall health, the patient’s response to the injection, and the type of injection used. Steroid injections may work well for some patients, while others may respond more positively to prolotherapy or PRP therapy.5Manchikanti L, Abdi S, Atluri S, Benyamin RM, Boswell MV, Buenaventura RM, et al. An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: Guidance and recommendations. Pain Physician. 2013;16(2 Suppl):S49-S283. https://pubmed.ncbi.nlm.nih.gov/23615883/
1-3 months post-injection
During the initial 3 months following the injection, many patients often experience significant relief from pain.1Foster ZJ, Voss TT, Hatch J, Frimodig A. Corticosteroid Injection for Common Musculoskeletal Conditions. Am Fam Physician. 2015;92(8):694-699. https://pubmed.ncbi.nlm.nih.gov/26554409/ The therapeutic injection enables them to engage in daily activities with less discomfort and participate in physical therapy or exercise to further improve their condition.
6 months post-injection
After 6 months, some patients continue to experience pain relief, but the injection’s effectiveness may diminish for others.6Kao MC, Chuang CW, Hung SK, Pan PT. Diagnosis and interventional pain management options for sacroiliac joint pain. Tzu Chi Medical Journal. 2019;31(4):207-210. Patients may begin to notice a return of their original pain around this time.
1-year post injection
One year after the injection, the effectiveness of the treatment has likely decreased for many patients. While some individuals may still benefit from ongoing pain relief, others may experience a recurrence of their pain.4D'Orazio F, Gregori LM, Gallucci M. Spine epidural and sacroiliac joints injections - when and how to perform. Eur J Radiol. 2015;84(5):777-782. http://doi:10.1016/j.ejrad.2014.05.039 At this stage, patients should consult their doctor to discuss the option of receiving another injection or exploring alternative treatment options.
It’s important to note that these are general trends and individual outcomes can vary. Some patients may experience longer-lasting pain relief, while others may have a shorter duration of relief.
Combining Other Treatments with SI Joint Injections
For increased overall effectiveness and treatment outcome, SI joint injections are often used in conjunction with other treatments, including4D'Orazio F, Gregori LM, Gallucci M. Spine epidural and sacroiliac joints injections - when and how to perform. Eur J Radiol. 2015;84(5):777-782. http://doi:10.1016/j.ejrad.2014.05.039:
- Physical therapy. Physical therapy can help strengthen the muscles around the SI joint, improve flexibility, and promote better posture, all of which can help reduce pain and prevent future injuries. The importance of physical therapy cannot be overstated. Patients who are not adequately guided to use correct posture and stretching techniques, typically continue to use the same movements that initially caused the pain.
While SI joint injections may provide temporary pain relief, they do not cure the underlying cause of pain. - Nonsteroidal anti-inflammatory drugs (NSAIDs): Over-the-counter NSAIDs, such as ibuprofen, can help reduce inflammation and pain.
- Heat and cold therapy. Applying heat or cold to the affected area can help reduce inflammation and pain.
It’s important to discuss these treatments with a doctor to determine which are appropriate for each patient’s underlying cause of SI joint pain.
- 1 Foster ZJ, Voss TT, Hatch J, Frimodig A. Corticosteroid Injection for Common Musculoskeletal Conditions. Am Fam Physician. 2015;92(8):694-699. https://pubmed.ncbi.nlm.nih.gov/26554409/
- 2 Cohen SP, Chen Y, Neufeld NJ. Sacroiliac Joint Pain: A Comprehensive Review of Epidemiology, Diagnosis and Treatment. Expert Rev Neurother. 2013;13(1):99-116. http://doi.org/10.1586/ern.12.148
- 3 Klauser A, Zordo TD, Feuchtner G, Sogner P, Schirmer M, Gruber J, Sepp N, Moriggl B. Feasibility of Ultrasound-Guided Sacroiliac Joint Injection Considering Sonoanatomic Landmarks at Two Different Levels in Cadavers and Patients. Arthritis & Rheumatism (Arthritis Care & Research). 2009, 59(11):1618-1624. http://doi.org/10.1002/art.24204
- 4 D'Orazio F, Gregori LM, Gallucci M. Spine epidural and sacroiliac joints injections - when and how to perform. Eur J Radiol. 2015;84(5):777-782. http://doi:10.1016/j.ejrad.2014.05.039
- 5 Manchikanti L, Abdi S, Atluri S, Benyamin RM, Boswell MV, Buenaventura RM, et al. An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: Guidance and recommendations. Pain Physician. 2013;16(2 Suppl):S49-S283. https://pubmed.ncbi.nlm.nih.gov/23615883/
- 6 Kao MC, Chuang CW, Hung SK, Pan PT. Diagnosis and interventional pain management options for sacroiliac joint pain. Tzu Chi Medical Journal. 2019;31(4):207-210.

