Percutaneous neuromodulation therapy (PNT) may be used as a complementary and alternative medicine treatment to manage back problems stemming from the musculoskeletal system. The treatment consists of electrical stimulation of a pain-transmitting nerve along its pathway in a muscle with the goal of altering or stopping the pain signals from reaching the brain and restoring function in the lower spine.
The terms percutaneous electrical nerve stimulation (PENS), electrical dry needling, or intramuscular electrical stimulation may be used interchangeably with PNT.1Fidalgo-Martin I, Ramos-Álvarez JJ, Murias-Lozano R, Rodríguez-López ES. Effects of percutaneous neuromodulation in neuromusculoskeletal pathologies: A systematic review. Medicine (Baltimore). 2022;101(41):e31016. doi:10.1097/MD.0000000000031016
Read more: All About Electrotherapy and Pain Relief
In This Article:
- Percutaneous Neuromodulation Therapy (PNT)
- Percutaneous Neuromodulation Therapy for Lower Back Pain
Specific Low Back Pain Conditions That May Benefit from PNT
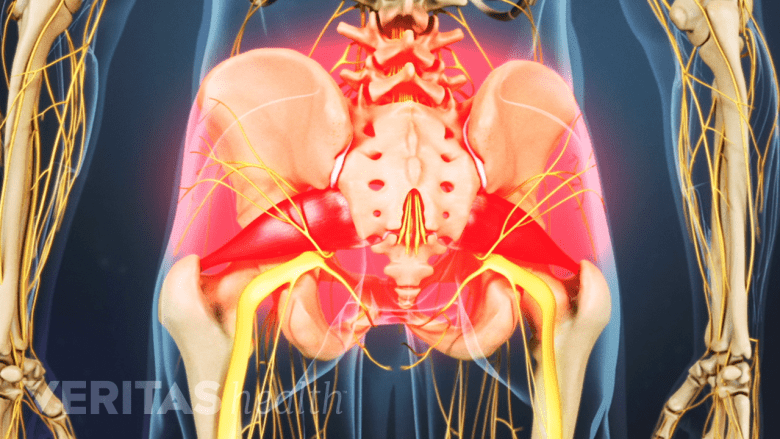
Percutaneous neuromodulation therapy benefits both acute and chronic axial back pain.
PNT may be recommended for patients with back pain who have not received adequate pain relief from nonsurgical treatments, such as physical therapy and/or pain medications. In these individuals, PNT may be added to the treatment regimen and performed along with physical therapy and/or other first-line treatments.
Specifically, the following back pain conditions may benefit from percutaneous neuromodulation therapy:
- Acute or chronic axial back pain: pain that is confined to the lower back region and does not radiate to the thigh or leg.2Cohen S, Gilmore C, Kapural L, et al. Percutaneous peripheral nerve stimulation for pain reduction and improvements in functional outcomes in chronic low back pain. Military Medicine. 2019;184(Supplement_1):537-541. doi:10.1093/milmed/usy310 Axial back pain is the most common type of low back pain and typically occurs due to muscle strains or ligament sprains.
- Chronic sciatica: pain and weakness caused by sciatic nerve root impingement in the lower back, with the symptoms radiating to the thigh, leg, and/or foot on the affected side. 3Ferreira‐Dos‐Santos G, Hurdle MFB, Gupta S, Clendenen SR. Ultrasound‐guided percutaneous peripheral nerve stimulation for the treatment of lower extremity pain: a rare case report. Pain Pract. 2019;19(8):861-865. doi:10.1111/papr.12810,4San-Emeterio-Iglesias R, Minaya-Muñoz F, Romero-Morales C, De-la-Cruz-Torres B. Correct sciatic nerve management to apply ultrasound-guided percutaneous neuromodulation in patients with chronic low back pain: a pilot study. Neuromodulation: Technology at the Neural Interface. 2021;24(6):1067-1074. doi:10.1111/ner.13396 The most common cause for sciatica is a herniated disc,5Kumar, Manish & Garg, Gaurav & Singh, L. & Singh, Talever & Tyagi, Lavi. (2011). Epidemiology, Pathophysiology and Symptomatic Treatment of Sciatica: A Review. International Journal of Pharmaceutical & Biological Archives. 2. 1050-1061. but other conditions such as degenerative disc disease and lumbar spinal stenosis may also cause sciatica.6Donnally III CJ, Varacallo M. Lumbar Degenerative Disk Disease. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448134/,7Valat J-P, Genevay S, Marty M, Rozenberg S, Koes B. Sciatica. Best Practice & Research Clinical Rheumatology. 2010;24(2):241-252. doi:10.1016/j.berh.2009.11.005. doi:https://doi.org/10.1016/j.berh.2009.11.005,8Ombregt L. The dural concept. In: A System of Orthopaedic Medicine. Elsevier; 2013:447-472.e4. doi:10.1016/b978-0-7020-3145-8.00033-8
- Acute or chronic post-surgical pain: pain and associated symptoms that develop after back surgery.2Cohen S, Gilmore C, Kapural L, et al. Percutaneous peripheral nerve stimulation for pain reduction and improvements in functional outcomes in chronic low back pain. Military Medicine. 2019;184(Supplement_1):537-541. doi:10.1093/milmed/usy310 Common causes of post-surgical back pain include psychosocial factors, long duration of surgery, inflammation of tissues during the surgical procedure, and nerve injury during surgery.9Wylde V, Dennis J, Beswick AD, et al. Systematic review of management of chronic pain after surgery. Br J Surg. 2017;104(10):1293-1306. doi:10.1002/bjs.10601
Back pain due to infections, cancer, or other medical emergencies is typically not treated with percutaneous neuromodulation therapy.
PNT Procedure for Low Back Pain Treatment

In PNT, paired needles are inserted into the skin from the mid-back to the buttock.
PNT is typically performed at a doctor’s office or physical therapy center. Patients can drive and resume physical activities after the procedure as sedation is not used for this treatment. The entire session may take 30 minutes to an hour depending on the area being treated and the dosage of electric current used.
- The patient lies on his/her stomach (prone position) or side and the skin over the treatment area is cleaned with an antiseptic solution.
- The needles are gently inserted into specific anatomic landmarks identified by the provider. The needle placement may begin at the mid-back region near the T12-L1 spinal segment (thoracolumbar joint) and continue all the way down to the buttock near the L5-S1 spinal segment (lumbosacral joint).10Seroussi RE, Gliner BE, Steinitz E, Schmitt S, Gamburd R, Firlik AD. Effectiveness of percutaneous neuromodulation therapy for patients with chronic and severe low back pain. Pain Practice. 2003;3(1):22-30. doi:10.1046/j.1533-2500.2003.00003.x
- The needles are inserted in pairs on either side of the spine and placed perpendicular to the skin’s surface. The needles used in PNT are hair-thin and do not cause pain when they are inserted into the skin. A depth of 2 cm to 5 cm is usually considered appropriate for PNT.11Fidalgo-Martin I, Ramos-Álvarez JJ, Murias-Lozano R, Rodríguez-López ES. Effects of percutaneous neuromodulation in neuromusculoskeletal pathologies: A systematic review. Medicine (Baltimore). 2022;101(41):e31016. doi:10.1097/MD.0000000000031016
- The needles are connected to wires, which are in turn connected to an electric device. Controlled electric current is passed through the device at a level that is tolerable to the patient without discomfort, pain, or visible muscle contractions. The frequency and dosage of electric current can be increased or decreased on the device. A mild tingling or tapping sensation may be felt when the electric current is passed through the needles.10Seroussi RE, Gliner BE, Steinitz E, Schmitt S, Gamburd R, Firlik AD. Effectiveness of percutaneous neuromodulation therapy for patients with chronic and severe low back pain. Pain Practice. 2003;3(1):22-30. doi:10.1046/j.1533-2500.2003.00003.x
- The session typically starts with a low-frequency electric current. If needed, the provider may change the frequency of electric current after a cycle of approximately 10 minutes.10Seroussi RE, Gliner BE, Steinitz E, Schmitt S, Gamburd R, Firlik AD. Effectiveness of percutaneous neuromodulation therapy for patients with chronic and severe low back pain. Pain Practice. 2003;3(1):22-30. doi:10.1046/j.1533-2500.2003.00003.x
After the treatment is complete, the needles are removed, and the patient may rest for a few minutes before resuming other activities. The skin over the treated area may be red or mildly irritated from the needle placement, which typically resolves the same day without treatment.
Number of PNT sessions needed for back pain treatment
Depending on the underlying cause of pain, the duration of PNT treatment may range from a few weeks up to 3 months. Sessions may range from 3 hours to 5 hours per week.12Doucet BM, Lam A, Griffin L. Neuromuscular electrical stimulation for skeletal muscle function. Yale J Biol Med. 2012;85(2):201-215. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3375668/
Some patients may experience pain relief after just a single PNT session, and some may experience little or no pain relief even after several sessions. The most appropriate frequency of treatments and course of therapy tend to vary for each patient.
Muscle Fatigue: A Potential Limitation of PNT
Some research suggests that repeated PNT treatment may cause muscle fatigue due to the following reasons12Doucet BM, Lam A, Griffin L. Neuromuscular electrical stimulation for skeletal muscle function. Yale J Biol Med. 2012;85(2):201-215. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3375668/:
- In normal muscle movement, the smaller muscle units are activated first, followed by the larger units. These smaller units are fatigue-resistant, which delays the onset of fatigue in the entire muscle. When electrically stimulated, all the muscle units get randomly activated, causing the onset of fatigue to occur sooner in PNT.
- PNT causes simultaneous, synchronized stimulation of muscle fibers, unlike a more random stimulation in normal circumstances, which causes more contractions, increasing overall muscle fatigue.
In some cases, the effectiveness of PNT may begin to wane following the discontinuation of treatment.
Electrical stimulation of muscles may help selective patients with back pain by improving muscle strength and blood flow, formation of healing tissue, and decreasing pain. Since the limitations, drawbacks, and side effects of this therapy are limited or rare, it may be considered for the treatment of back pain in patients who are hesitant to try more invasive injection treatments or consider surgery for pain relief.
- 1 Fidalgo-Martin I, Ramos-Álvarez JJ, Murias-Lozano R, Rodríguez-López ES. Effects of percutaneous neuromodulation in neuromusculoskeletal pathologies: A systematic review. Medicine (Baltimore). 2022;101(41):e31016. doi:10.1097/MD.0000000000031016
- 2 Cohen S, Gilmore C, Kapural L, et al. Percutaneous peripheral nerve stimulation for pain reduction and improvements in functional outcomes in chronic low back pain. Military Medicine. 2019;184(Supplement_1):537-541. doi:10.1093/milmed/usy310
- 3 Ferreira‐Dos‐Santos G, Hurdle MFB, Gupta S, Clendenen SR. Ultrasound‐guided percutaneous peripheral nerve stimulation for the treatment of lower extremity pain: a rare case report. Pain Pract. 2019;19(8):861-865. doi:10.1111/papr.12810
- 4 San-Emeterio-Iglesias R, Minaya-Muñoz F, Romero-Morales C, De-la-Cruz-Torres B. Correct sciatic nerve management to apply ultrasound-guided percutaneous neuromodulation in patients with chronic low back pain: a pilot study. Neuromodulation: Technology at the Neural Interface. 2021;24(6):1067-1074. doi:10.1111/ner.13396
- 5 Kumar, Manish & Garg, Gaurav & Singh, L. & Singh, Talever & Tyagi, Lavi. (2011). Epidemiology, Pathophysiology and Symptomatic Treatment of Sciatica: A Review. International Journal of Pharmaceutical & Biological Archives. 2. 1050-1061.
- 6 Donnally III CJ, Varacallo M. Lumbar Degenerative Disk Disease. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448134/
- 7 Valat J-P, Genevay S, Marty M, Rozenberg S, Koes B. Sciatica. Best Practice & Research Clinical Rheumatology. 2010;24(2):241-252. doi:10.1016/j.berh.2009.11.005. doi:https://doi.org/10.1016/j.berh.2009.11.005
- 8 Ombregt L. The dural concept. In: A System of Orthopaedic Medicine. Elsevier; 2013:447-472.e4. doi:10.1016/b978-0-7020-3145-8.00033-8
- 9 Wylde V, Dennis J, Beswick AD, et al. Systematic review of management of chronic pain after surgery. Br J Surg. 2017;104(10):1293-1306. doi:10.1002/bjs.10601
- 10 Seroussi RE, Gliner BE, Steinitz E, Schmitt S, Gamburd R, Firlik AD. Effectiveness of percutaneous neuromodulation therapy for patients with chronic and severe low back pain. Pain Practice. 2003;3(1):22-30. doi:10.1046/j.1533-2500.2003.00003.x
- 12 Doucet BM, Lam A, Griffin L. Neuromuscular electrical stimulation for skeletal muscle function. Yale J Biol Med. 2012;85(2):201-215. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3375668/

