Posterior lumbar interbody fusion (PLIF) aims to fuse two levels of the spine by taking a surgical approach from behind the lumbar spine.
Specifically, the abbreviation PLIF stands for:
- Posterior, meaning from the back
- Lumbar, referring to the lumbar spine in the lower back
- Interbody, meaning the area between two adjacent vertebral bones in the spine
- Fusion, referring to the process of two bones becoming one
The spinal disc between the two vertebral bodies is removed, then replaced with a cage made of either allograft bone or synthetic material (such as titanium). A biological response causes the bone to grow between the two vertebral elements and thereby stops the motion at that segment.
In most cases, a PLIF fusion is supplemented by a simultaneous posterolateral spine fusion (PLF) surgery.1Plantz MA, Hsu WK. Single-level Posterolateral Fusion (PLF) Alone and Posterior Interbody Fusion (PLIF/TLIF) Alone Lead to a Decreased Risk of Short-term Complications Compared to Combined PLF With PLIF/TLIF Procedures: A Matched Analysis. Spine (Phila Pa 1976). 2020;45(21):E1391-E1399. doi:10.1097/BRS.0000000000003615
In This Article:
- Posterior Lumbar Interbody Fusion (PLIF) Surgery
- PLIF Potential Advantages and Disadvantages
- Posterior Lumbar Interbody Fusion (PLIF) Video
Posterior Lumbar Interbody Fusion Surgery: Step-by-Step Description
PLIF surgery uses cages to fill disc space with bone grafts, facilitating spinal fusion.
A PLIF surgery is performed by a spine surgeon in a hospital setting or an outpatient surgery center.
The surgery typically lasts about 2 to 6 hours, based on a number of factors such as the surgeon’s experience with this type of surgery, the patient’s overall health, any co-existing conditions such as spondylolisthesis, and the number of spinal levels involved.
The steps of a typical open PLIF surgery include:
- The spine is approached through a 3-inch to 6-inch incision in the midline of the back, creating access to one or two levels of the spine. The left and right lower back muscles (erector spinae) are dissected off the lamina on both sides and at multiple levels. Typically, the exposure will include visualization of the spinous process, lamina, facet joints, and transverse process for each vertebral level involved. For example, a PLIF at the L4-L5 spinal segment would include exposure of the L4 spinous process and lamina, the L4-L5 and L3-L4 facet joints, and the transverse processes of the L4 and L5 vertebrae.
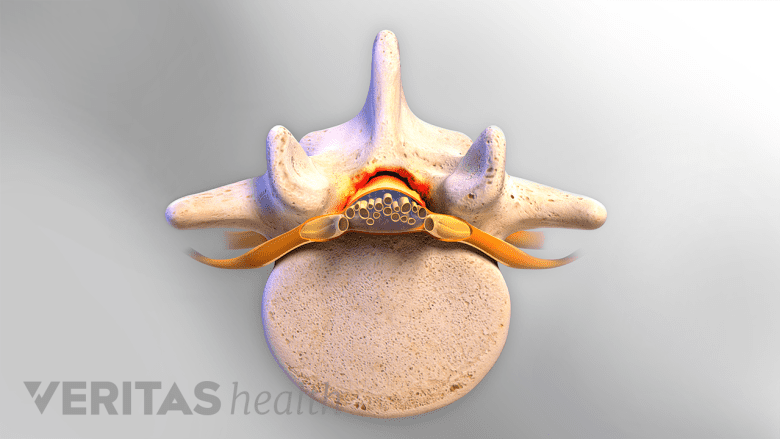
- The spinous process of the involved level is removed, followed by the removal of one or more laminae (laminectomy) to allow decompression and visualization of the thecal sac and dura in the midline and the exiting nerve roots on both sides. The facet joints, which are directly over the nerve roots, may then be undercut (trimmed) to give the nerve roots more room.
- The nerve roots are then gently retracted to the midline to access the posterior disc annulus. The annulus is incised and the disc material is removed. The disc plates are prepared to create the necessary fusion environment. This procedure is repeated on the other side of the disc. The space created on each side is intended for the insertion of interbody implants and the bone graft material.
- Instrumentation includes the placement of two interbody spacers in combination with bone graft into the disc space. Screws are placed bilaterally (on both the left and the right sides) above and below the fused vertebrae, then connected with small metal rods to help stabilize the vertebral bodies as the fusion occurs. The bone grows from the vertebral body of one level to the vertebral body of the other level.
After surgery, it is typical to remain in the hospital for at least one day before returning home, but in some cases, the patient may return home the same day. The patient may feel immediate relief from presurgical pain or the pain may resolve gradually as the body recovers from surgery.
Read more about Postoperative Care for Spinal Fusion Surgery
The surgeon provides postoperative instructions that typically include rest and physical therapy to help with recovery. Activities increase as the recovery proceeds. The surgeon will take an x-ray image of the fused levels to ensure that the bone has become one. While the process of bony fusion begins to take place at around 6 weeks, bone remodeling and fusion typically become stronger over a full year.2Ushirozako H, Hasegawa T, Ebata S, et al. Impact of Early Intervertebral Osseous Union After Posterior Lumbar Interbody Fusion on Health-Related Quality of Life. Global Spine J. 2022;12(3):399-408. doi:10.1177/2192568220953813,3Hasegawa T, Ushirozako H, Shigeto E, et al. The Titanium-coated PEEK Cage Maintains Better Bone Fusion With the Endplate Than the PEEK Cage 6 Months After PLIF Surgery: A Multicenter, Prospective, Randomized Study. Spine (Phila Pa 1976). 2020;45(15):E892-E902. doi:10.1097/BRS.0000000000003464
Watch Video: Stages of Bone Healing in Lumbar Spine Fusion Surgery
PLIF Surgery Variations
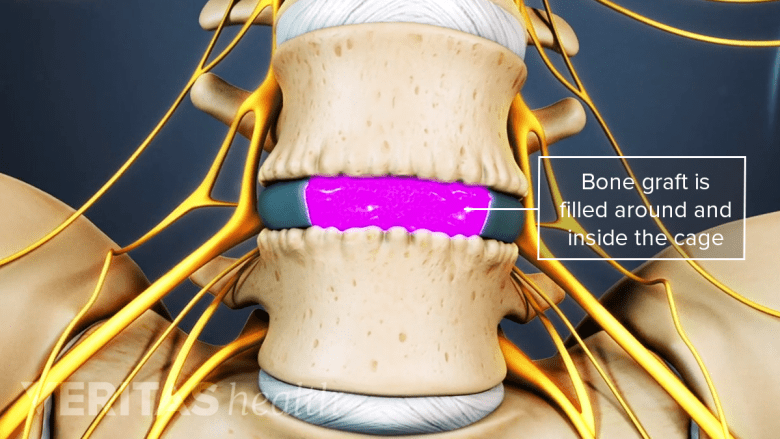
Bone grafts are typically used in PLIF surgery to promote spinal fusion and stability.
There are a number of variations to the posterior lumbar interbody fusion, including but not limited to:
- Minimally invasive approach. An alternative to the conventional open-spine surgery is minimally invasive spine surgery, which uses one to two smaller incisions and may reduce the need to disrupt the back muscles. Notable advantages of the minimally invasive approach may include reduced blood loss and a reduction in postsurgical incisional pain.4Imada AO, Huynh TR, Drazin D. Minimally Invasive Versus Open Laminectomy/Discectomy, Transforaminal Lumbar, and Posterior Lumbar Interbody Fusions: A Systematic Review. Cureus. 2017;9(7):e1488. Published 2017 Jul 18. doi:10.7759/cureus.1488,5Makanji H, Schoenfeld AJ, Bhalla A, Bono CM. Critical analysis of trends in lumbar fusion for degenerative disorders revisited: influence of technique on fusion rate and clinical outcomes. Eur Spine J. 2018;27(8):1868-1876. doi:10.1007/s00586-018-5544-x Disadvantages may include limited visualization for adequate nerve decompression and preparation of fusion services. Another minimally invasive step may be taken during screw fixation, by using a cortical bone trajectory screw as opposed to the traditional pedicle screw.6Sakaura H, Miwa T, Yamashita T, Kuroda Y, Ohwada T. Posterior lumbar interbody fusion with cortical bone trajectory screw fixation versus posterior lumbar interbody fusion using traditional pedicle screw fixation for degenerative lumbar spondylolisthesis: a comparative study. J Neurosurg Spine. 2016;25(5):591-595. doi:10.3171/2016.3.SPINE151525
- Robotics. PLIF surgery can be performed freehand or with robotic techniques, which are most useful in minimally invasive approaches and when there are anatomical challenges, such as scoliosis. Robot-guided PLIF helps the surgeon to drill the pedicle screw using a precise position and trajectory.7Joseph JR, Smith BW, Liu X, Park P. Current applications of robotics in spine surgery: a systematic review of the literature. Neurosurg Focus. 2017;42(5):E2. doi:10.3171/2017.2.FOCUS16544
- Type of bone graft. Bone graft(s) can be obtained from the patient, a cadaver, or manufactured substitutes. Different bone graft materials can also be used in conjunction; for example, a bone graft may be obtained from a cadaver and combined with liquid bone marrow from the patient.
- Use of bone morphogenetic proteins (BMPs). One of the BMPs, recombinant human bone morphogenetic protein-2 (rhBMP-2), can be used as a bone graft substitute. This regenerative protein is combined with ceramic and/or polymer composites to make the bone graft substitute easy to handle and mechanically strong. While BMPs may be used in many approaches to spinal fusion surgery, they are only FDA-approved in anterior lumbar interbody fusion (ALIF).
- Type of interbody cage. Cages are available in several materials, sizes, and designs. For example, a cage may be made of the thermoplastic polymer PEEK, coated with titanium, and shaped as a cylinder. Because PLIF usually removes disc material on both sides, two cages are often used to fill the interbody space with bone grafts. All interbody cages are designed to have pores, allowing bone to grow through the openings during fusion.
- Simultaneous procedures. A PLIF surgery fuses two vertebral bodies and it can be combined with a posterolateral fusion (PLF) surgery, which fuses other parts of the spine, such as the transverse processes. Having simultaneous procedures for spinal fusion may increase the risk of short-term complications.1Plantz MA, Hsu WK. Single-level Posterolateral Fusion (PLF) Alone and Posterior Interbody Fusion (PLIF/TLIF) Alone Lead to a Decreased Risk of Short-term Complications Compared to Combined PLF With PLIF/TLIF Procedures: A Matched Analysis. Spine (Phila Pa 1976). 2020;45(21):E1391-E1399. doi:10.1097/BRS.0000000000003615
The above considerations rely on a number of factors such as the patient’s specific diagnosis and overall health, and the surgeon’s experience and preference.
PLIF Surgery Indications
Spinal stenosis is an indication for PLIF surgery.
Severe lower back pain combined with neurological symptoms of leg pain that persist despite months of nonsurgical treatments may lead to the consideration of PLIF as a surgical treatment. Conditions that may cause such severe pain include8Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2-18. doi:10.3978/j.issn.2414-469X.2015.10.05:
- Degenerative disc disease with spinal instability
- Recurrent disc herniation
- Spondylolisthesis
- Spinal stenosis
- Pseudoarthrosis from a prior spinal fusion surgery that did not result in a fusion
The posterior approach used in PLIF surgery is favored for up to 2 vertebral levels that need to be fused using laminectomy (a method of decompression) and instrumentation (the use of metal rods and screws). PLIF is less preferred when the levels to be fused include L1 and/or L2 because the spinal cord can be more difficult to retract in the region of the lumbar spine that is closer to the mid-back region.
PLIF Surgery Contraindications
Spinal fusion surgery may not be recommended when there is a history of multiple back surgeries and extensive scarring from such surgeries or injuries. Other common contraindications to PLIF and other types of spinal fusion include an active infection or arachnoiditis (inflammation in the spinal canal).
PLIF Surgery Is a Traditional Approach
PLIF surgery is one of the earliest approaches to spinal fusion, so this approach is tried and tested with many decades of technological advancements. Several procedures allow PLIF to be minimally invasive. Another type of fusion surgery similar to PLIF is transforaminal lumbar interbody fusion (TLIF), which takes an approach from the side and decreases the risk of nerve injury. It is important to consider the surgeon’s level of experience with PLIF and discuss the risks and benefits of the posterior approach.
- 1 Plantz MA, Hsu WK. Single-level Posterolateral Fusion (PLF) Alone and Posterior Interbody Fusion (PLIF/TLIF) Alone Lead to a Decreased Risk of Short-term Complications Compared to Combined PLF With PLIF/TLIF Procedures: A Matched Analysis. Spine (Phila Pa 1976). 2020;45(21):E1391-E1399. doi:10.1097/BRS.0000000000003615
- 2 Ushirozako H, Hasegawa T, Ebata S, et al. Impact of Early Intervertebral Osseous Union After Posterior Lumbar Interbody Fusion on Health-Related Quality of Life. Global Spine J. 2022;12(3):399-408. doi:10.1177/2192568220953813
- 3 Hasegawa T, Ushirozako H, Shigeto E, et al. The Titanium-coated PEEK Cage Maintains Better Bone Fusion With the Endplate Than the PEEK Cage 6 Months After PLIF Surgery: A Multicenter, Prospective, Randomized Study. Spine (Phila Pa 1976). 2020;45(15):E892-E902. doi:10.1097/BRS.0000000000003464
- 4 Imada AO, Huynh TR, Drazin D. Minimally Invasive Versus Open Laminectomy/Discectomy, Transforaminal Lumbar, and Posterior Lumbar Interbody Fusions: A Systematic Review. Cureus. 2017;9(7):e1488. Published 2017 Jul 18. doi:10.7759/cureus.1488
- 5 Makanji H, Schoenfeld AJ, Bhalla A, Bono CM. Critical analysis of trends in lumbar fusion for degenerative disorders revisited: influence of technique on fusion rate and clinical outcomes. Eur Spine J. 2018;27(8):1868-1876. doi:10.1007/s00586-018-5544-x
- 6 Sakaura H, Miwa T, Yamashita T, Kuroda Y, Ohwada T. Posterior lumbar interbody fusion with cortical bone trajectory screw fixation versus posterior lumbar interbody fusion using traditional pedicle screw fixation for degenerative lumbar spondylolisthesis: a comparative study. J Neurosurg Spine. 2016;25(5):591-595. doi:10.3171/2016.3.SPINE151525
- 7 Joseph JR, Smith BW, Liu X, Park P. Current applications of robotics in spine surgery: a systematic review of the literature. Neurosurg Focus. 2017;42(5):E2. doi:10.3171/2017.2.FOCUS16544
- 8 Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2-18. doi:10.3978/j.issn.2414-469X.2015.10.05

