The principal risk of any spinal fusion surgery is that a solid fusion will not be obtained (nonunion). As with most spinal surgeries, an additional risk is lack of, or insufficient, pain relief for the patient. Risks and complications from the anterior lumbar interbody fusion (ALIF) approach tend to be relatively rare, reversible, and/or fleeting.

Rarely, nerve damage may occur as a complication of ALIF surgery.
The majority of the known complications are related to the surgical approach from the front, which crosses or bypasses layers of fat and muscles, internal organs, nerves, and blood vessels.
In This Article:
- Anterior Lumbar Interbody Fusion (ALIF) Surgery
- Potential Risks and Complications with ALIF Surgery
- ALIF (Anterior Lumbar Interbody Fusion) Video
Constipation or Difficulty Eating After Surgery
Temporary constipation and/or dietary changes may occur during recovery in the days immediately following surgery. Around 3 days after ALIF, patients may experience post-operative ileus, or constipation–a typical postoperative issue after abdominal surgery. This issue translates to an inability to eat solid food. This complication occurs in about 3% of ALIF patients,1Manunga J, Alcala C, Smith J, et al. Technical approach, outcomes, and exposure-related complications in patients undergoing anterior lumbar interbody fusion. J Vasc Surg. 2021;73(3):992-998. doi:10.1016/j.jvs.2020.06.129 but soon resolves on its own.
See Preventing Constipation After Back Surgery
Infection or Incisional Hernia
The incision made when performing ALIF surgery takes months of relative rest to heal fully. Without attentive care and rest, complications can occur. In about 2.6% of patients, the site of incision can become infected or, rarely, develop a hernia.1Manunga J, Alcala C, Smith J, et al. Technical approach, outcomes, and exposure-related complications in patients undergoing anterior lumbar interbody fusion. J Vasc Surg. 2021;73(3):992-998. doi:10.1016/j.jvs.2020.06.129
An incisional hernia occurs when the tissues of the abdominal lining begin to protrude outward and can be described as a lump or a bulge that may be more pronounced with activity. Standard treatment for a hernia is surgery to put the tissue back in place. An additional step to insert a surgical mesh may be needed to prevent the tissue from protruding again.
Retrograde Ejaculation in Males
A risk unique to males is a condition known as retrograde ejaculation. Approaching the L5-S1 (lumbar segment 5 and sacral segment 1) disc space from the front creates this risk. The small nerves directly over the disc interspace control a valve that causes the ejaculate to be expelled during intercourse.
Dissection over the disc space may cause the nerves to stop working, forcing the ejaculate to take the path of least resistance, which is up into the bladder. Retrograde ejaculation happens in about 2% of cases and tends to resolve between 3 months to 4 years after surgery.2Body AM, Plummer ZJ, Krueger BM, et al. Retrograde ejaculation following anterior lumbar surgery: a systematic review and pooled analysis. J Neurosurg Spine. 2021;35(4):427-436. Published 2021 Jul 16. doi:10.3171/2020.12.SPINE201101
With retrograde ejaculation, the sensation of ejaculating is largely the same. Conception can become difficult, but this complication does not result in impotence because these nerves do not control erection. A surgeon may consider other approaches to spinal fusion surgery, such as PLIF, for younger male patients.
Bowel Obstruction or Abdominal Pain
Injury to the bowel or other bowel complications are infrequent, occurring in as little as 0.25% of surgeries.1Manunga J, Alcala C, Smith J, et al. Technical approach, outcomes, and exposure-related complications in patients undergoing anterior lumbar interbody fusion. J Vasc Surg. 2021;73(3):992-998. doi:10.1016/j.jvs.2020.06.129 During ALIF surgery, the peritoneum (a large sack that holds the internal organs) may experience a rupture or abrasion, known as a serosal tear. Small serosal tears can be repaired during surgery, using absorbable or permanent stitches.
Blood flow to the intestines may be limited if a blood clot (embolism) lodges into one of the supplying arteries. If this complication occurs, a patient may experience abdominal pain that gets worse after a meal. Treatment options for interrupted blood flow to the bowel include blood thinning medications or surgery.
Such injuries occur in about 1.4% of cases.1Manunga J, Alcala C, Smith J, et al. Technical approach, outcomes, and exposure-related complications in patients undergoing anterior lumbar interbody fusion. J Vasc Surg. 2021;73(3):992-998. doi:10.1016/j.jvs.2020.06.129
Deep Vein Thrombosis After ALIF Surgery
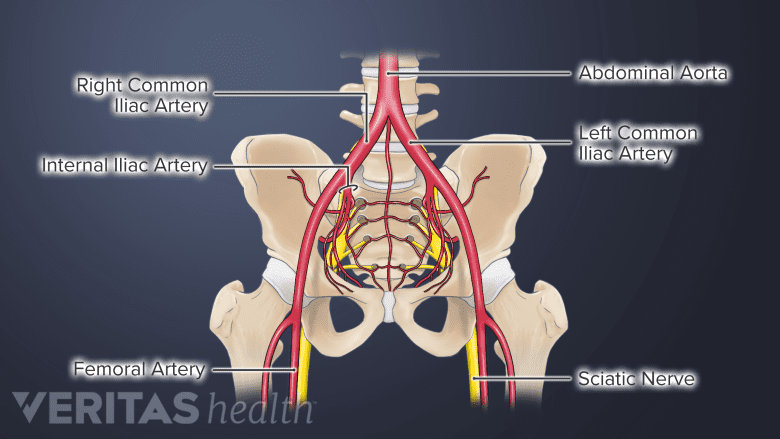
The anterior approach can result in vascular complications due to its proximity to critical blood vessels and arteries.
Risk of deep vein thrombosis (DVT) occurs in up to 14% of cases,3Vint H, Mawdsley MJ, Coe C, Jensen CD, Kasis AG. The Incidence of Venous Thromboembolism in Patients Undergoing Anterior Lumbar Interbody Fusion: A Proposed Thromboprophylactic Regime. Int J Spine Surg. 2021;15(2):348-352. doi:10.14444/8045 and is higher in individuals who have been diagnosed with iliac vein compression syndrome, also known as May-Thurner syndrome. The syndrome involves the compression of the left iliac vein, between the L5 vertebrae and the right iliac artery. About 22% of people are expected to have this anatomical compression,4Reddy D, Mikhael MM, Shapiro GS, Farrell T. Extensive Deep Venous Thrombosis Resulting from Anterior Lumbar Spine Surgery in a Patient with Iliac Vein Compression Syndrome: A Case Report and Literature Review. Global Spine J. 2015;5(4):e22-e27. doi:10.1055/s-0034-1396431 which may or may not lead to DVT during one’s lifetime.
Blood Loss After ALIF Surgery
ALIF is performed in close proximity to the large blood vessels that go to the legs, creating the risk of vascular problems, such as blood loss or injured blood vessels.
The total blood lost is measured by calculating the estimated volume of blood loss during surgery and the hemoglobin level of the blood after surgery. The difference between the total blood lost and the estimated blood lost is called hidden blood loss, which makes up about 40% of the total blood lost in both anterior and posterior approaches to surgery.5Ju H, Hart RA. Hidden blood loss in anterior lumbar interbody fusion (ALIF) surgery. Orthop Traumatol Surg Res. 2016;102(1):67-70. doi:10.1016/j.otsr.2015.10.003 Hidden blood loss may contribute to prolonged hospitalization and recovery.
This potential risk of damage to veins or arteries is an uncommon complication in the hands of experienced vascular and spine surgeons.
Other ALIF Considerations
In general, the principal risk of this type of spine surgery is that a solid fusion will not be obtained (nonunion) and further surgery to re-fuse the spine may be necessary. Fusion rates for an ALIF are typically as high as 90% to 95%.6Manzur M, Virk SS, Jivanelli B, et al. The rate of fusion for stand-alone anterior lumbar interbody fusion: a systematic review. Spine J. 2019;19(7):1294-1301. doi:10.1016/j.spinee.2019.03.001
Nonunion rates are higher for patients who:
- Have had prior lower back surgery
- Smoke or are obese
- Have multiple level fusion surgery
- Have been treated with radiation for cancer
Not all patients who have a nonunion will need to have another fusion procedure. As long as the joint is stable and the patient's symptoms are better, more back surgery is not necessary.
See Spine Fusion Risks and Complications
In addition, there is a risk that the patient’s back pain does not subside, despite achieving a successful fusion. For more information, see Failed Back Surgery Syndrome.
- 1 Manunga J, Alcala C, Smith J, et al. Technical approach, outcomes, and exposure-related complications in patients undergoing anterior lumbar interbody fusion. J Vasc Surg. 2021;73(3):992-998. doi:10.1016/j.jvs.2020.06.129
- 2 Body AM, Plummer ZJ, Krueger BM, et al. Retrograde ejaculation following anterior lumbar surgery: a systematic review and pooled analysis. J Neurosurg Spine. 2021;35(4):427-436. Published 2021 Jul 16. doi:10.3171/2020.12.SPINE201101
- 3 Vint H, Mawdsley MJ, Coe C, Jensen CD, Kasis AG. The Incidence of Venous Thromboembolism in Patients Undergoing Anterior Lumbar Interbody Fusion: A Proposed Thromboprophylactic Regime. Int J Spine Surg. 2021;15(2):348-352. doi:10.14444/8045
- 4 Reddy D, Mikhael MM, Shapiro GS, Farrell T. Extensive Deep Venous Thrombosis Resulting from Anterior Lumbar Spine Surgery in a Patient with Iliac Vein Compression Syndrome: A Case Report and Literature Review. Global Spine J. 2015;5(4):e22-e27. doi:10.1055/s-0034-1396431
- 5 Ju H, Hart RA. Hidden blood loss in anterior lumbar interbody fusion (ALIF) surgery. Orthop Traumatol Surg Res. 2016;102(1):67-70. doi:10.1016/j.otsr.2015.10.003
- 6 Manzur M, Virk SS, Jivanelli B, et al. The rate of fusion for stand-alone anterior lumbar interbody fusion: a systematic review. Spine J. 2019;19(7):1294-1301. doi:10.1016/j.spinee.2019.03.001
Editor’s Top Picks
- ALIF (Anterior Lumbar Interbody Fusion) Video
- Spine Fusion Risks and Complications
- Failed Back Surgery Syndrome (FBSS): What It Is and How to Avoid Pain after Surgery
- Postoperative Care for Spinal Fusion Surgery
- Video: Stages of Bone Healing in Lumbar Spine Fusion Surgery
- L5-S1 Anterior Lumbar Interbody Fusion Surgery Animation

