Because osteoporosis is a "silent" disease, meaning that there are typically no symptoms until a fracture occurs, it is not uncommon for someone with back pain to be unaware of the fact that he or she has actually fractured a vertebra (or multiple vertebrae) in their spine.
In This Article:
Typical Compression Fracture Symptoms
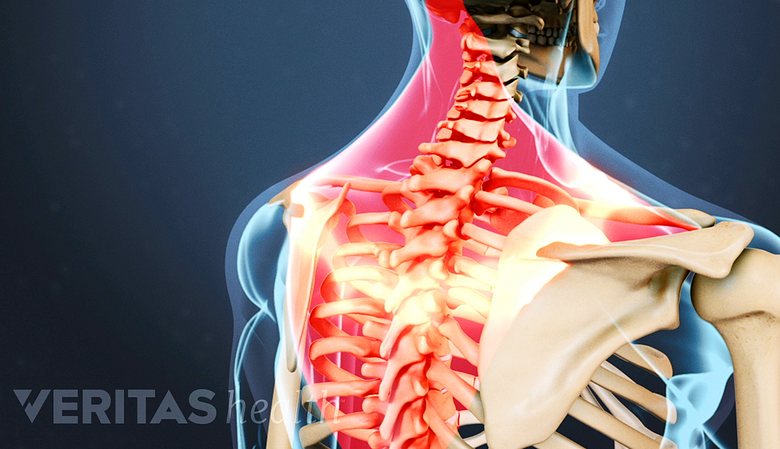
Sudden onset of back pain is a common symptom of vertebral fractures.
The main clinical symptoms of vertebral fractures typically include one or a combination of the following symptoms:
- Sudden onset of back pain
- Standing or walking will usually make the pain worse
- Lying on one's back makes the pain less intense
- Limited spinal mobility
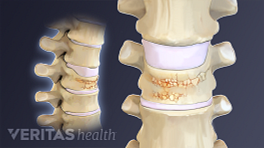
- Height loss
- Deformity and disability
As a general rule, a compression fracture should be suspected in any patient over the age of 50 with acute onset of back pain. For women, especially those with risk factors for osteoporosis, many physicians believe that a vertebral fracture should be suspected in any women over age 45 with sudden onset of back pain.
See Who Is at Risk for Osteoporosis?
Sometimes a compression fracture in the spine may not cause any back pain or other symptoms. Therefore, even if there is not back pain, middle age or elderly persons (especially women) need to be concerned about potential fractures if there is height loss, limited ability to twist and bend the back, and/or deformity that develops in the spine.
Typical Progression of Compression Fracture Symptoms
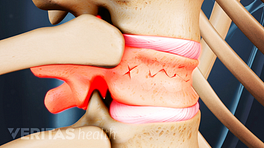
When osteoporosis results in a vertebral fracture, it is usually marked by the sudden onset of back pain. Most patients diagnosed with a compression fracture in the spine describe the onset of pain immediately after a fairly routine activity that slightly strains or jars the back, such as:
- Lifting - opening a window or picking up a bag of groceries
- Bending - picking something up off the floor
- Falling - jarring the spine by missing a step or slipping on ice.
For people with advanced osteoporosis, the fracture can even occur with extremely minor activity, such as sneezing, coughing, getting in or out of the bathtub, or simply turning over in bed. The pain from an osteoporotic spinal fracture typically lasts about four to six weeks as the bone heals, after which most patients report that the more severe pain has subsided and has turned into more of a chronic, achy pain concentrated in the area of the back where the fracture occurred.
This pain will usually get better after a few weeks, but for some people it can continue for several months. Additionally, some patients experience back pain long after the fractured bone has healed due to changed mechanics in the back and possibly due to inactivity.
Other Types of Fracture Pain Patterns
The above describes the course of events that is experienced by most patients with a vertebral compression fracture. However, not everyone has a typical experience. Examples of other types of pain patterns include:
- If the bone collapses gradually rather than due to an activity, the pain will usually be more gradual and mild.
- Some patients with vertebral fractures report that they felt no back pain or other symptoms.
- For others, instead of pain the symptoms of deformity that start to show up after multiple fractures may be the patient's first indication that he or she has vertebral fractures from osteoporosis.
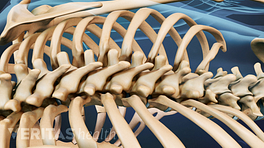
Multiple Compression Fractures
Unlike many other conditions that can be treated before a serious complication develops, usually a fracture is the first sign that someone has osteoporosis. By the time a fracture occurs, the osteoporosis is usually advanced and the individual is then at risk for sustaining more vertebral fractures.