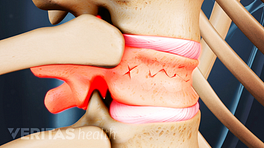
It is important to accurately diagnose vertebral compression fractures due to osteoporosis, as there are a number of potential adverse effects if a diagnosis is missed and there is no treatment. In general, vertebral fractures are associated with both increased morbidity (unwanted side effects) and mortality (death).
- Morbidity (side effects) associated with vertebral fractures often includes continued pain, decreased physical function, deformity, and potentially social isolation, all of which negatively impact the individual's overall quality of and enjoyment of life.
- Mortality is also associated with vertebral fractures, as women diagnosed with a compression fracture of the spine have a 15% higher mortality rate than those who do not experience fractures. 1 Riggs, B.L. and L.J. Melton, 3rd, "The worldwide problem of osteoporosis: insights afforded by epidemiology," Bone, 1995, 17(5 Suppl): p. 505S-511S.
The presence of one vertebral fracture increases the risk of any subsequent vertebral fracture 5-fold. Of women who have had a recent vertebral fracture, it is estimated that approximately 20% will sustain a new fracture within the next 12 months.
In This Article:
- When Back Pain Is a Spine Compression Fracture
- Vertebral Fracture Symptoms
- Osteoporosis: The Primary Cause of Collapsed Vertebrae
- Diagnosing Vertebral Compression Fractures
- Compression Fracture Treatment
Difficulty in Diagnosing an Osteoporosis Fracture
Unlike many other conditions, diagnosing a vertebral compression fracture is not as straightforward as one would think. For example:
- When an elderly person complains of back pain, it is often assumed to be just general back pain, spinal arthritis, or a normal part of the aches and pains associated with aging. This assumption may be made by the patient, by his or her family or caregivers, and/or by the treating physician. When this happens, the patient is often not even checked for a vertebral fracture.
- In most cases of an osteoporosis-related hip or wrist fracture, the fractured bone is easily identified by a standard x-ray. However, in the spine a compression fracture may be missed on an x-ray, and if this is the case it may be assumed that the patient's pain is due to general muscle strain or just the aches and pains that accompany aging.
For these and other reasons, it is estimated that only about one-third of vertebral compression fractures that occur in the U.S. each year are diagnosed.
Diagnostic Process
The diagnostic process includes a complete history of the patient's condition, medical history, and family history. A number of questions related to the patient’s pain will probably be asked, such as:
- When did the pain start? Was it sudden or gradual?
- Where is the pain? What is the intensity of the pain?
- What activities or positions tend to make the pain feel better or worse?
- Does the pain radiate down the leg or arm or to other parts of the body?
After taking the patient's history, the physician will do a physical examination, with the objective of trying to determine the cause of the pain and ruling out other possible problems.
If a vertebral compression fracture is suspected, the doctor will test for tenderness and sensitivity near specific vertebrae along the spine. Based on the patient's history and physical exam, if a vertebral fracture is suspected, an x-ray will be ordered to confirm the diagnosis.
Diagnostic Tests
MRI scans offer detailed views of soft tissues, including nerves and discs around the fracture.
Depending on the physician's findings from the patient's history, physical exam, and x-ray, additional diagnostic tests may also be needed, such as:
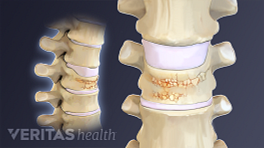
- A CAT scan, to see whether or not the fractured bone is stable and/or to see if the adjacent nerves near the fracture are being irritated or may be affected by the fracture. Because a CAT scan can show soft tissue (e.g. nerves) as well as bone, and because it can take cross-sectional images of the spine, it provides the physician more information than an x-ray.
- An MRI scan may be ordered if the doctor suspects that there may be some other cause of the patient’s pain (e.g. a herniated disc), or if there is a chance that nerves near the fracture are affected. An MRI scan shows a high level of detail of the soft tissues (e.g. nerves, discs) surrounding the fracture that may be affected. An MRI scan can also tell if the fracture is old or new. In a new fracture the bone will be particularly dark on one sequence of films (the T1 weighted sagittal images).
- A nuclear bone scan may be used to help determine when the fracture occurred. The age of the fracture is sometimes important to know to help guide treatment options.
- 1 Riggs, B.L. and L.J. Melton, 3rd, "The worldwide problem of osteoporosis: insights afforded by epidemiology," Bone, 1995, 17(5 Suppl): p. 505S-511S.