Osteoarthritis occurs when the protective cartilage in a joint begins to break down and no longer facilitates smooth movement between bones, which can eventually result in the joint becoming swollen and painful. When this condition develops in the cervical spine, it is called cervical osteoarthritis.
Sometimes confusion is created when general terms are used interchangeably to refer to cervical osteoarthritis, including cervical spondylosis, degenerative joint disease, or simply neck arthritis. On this site, cervical osteoarthritis is the term that specifically describes the degeneration of the facet joints in the cervical spine.
In This Article:
- Cervical Osteoarthritis (Neck Arthritis)
- Cervical Osteoarthritis Symptoms
- Diagnosing Cervical Osteoarthritis
- Cervical Osteoarthritis Treatment
- Cervical Facet Osteoarthritis Video
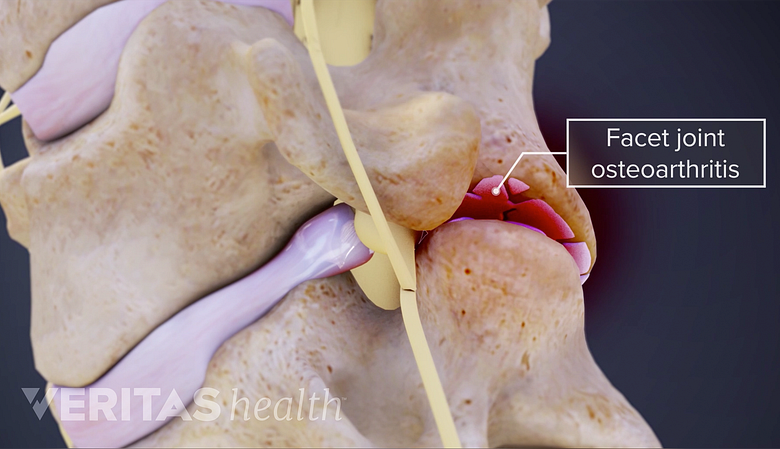
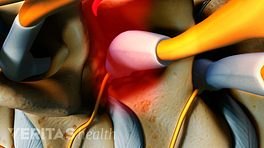
The Facet Joint and What Can Go Wrong
Facet joint arthritis involves the degeneration and inflammation of the spine's facet joints, leading to pain and reduced mobility.
The facet joints, also called zygapophysial joints, are a key part of the spine’s flexibility. Two small facet joints are located at the back of each vertebral level (one to the right and one to the left), enabling limited forward/backward and twisting motion. In the cervical spine, these joints are called cervical facet joints.
A facet joint is comprised of hard yet smooth cartilage on the upper and lower articulating surfaces to protect the back part of vertebral bones. The joint is encased in a protective capsule, and inside this capsule is synovial fluid which provides the lubrication for smooth movements.
When the cartilage starts to wear away, bone starts rubbing against bone, which can facilitate excessive bone growth, known as bone spurs (osteophytes). Bone rubbing against bone can cause inflammation and pain. Furthermore, fragments of bone and cartilage might break off and start floating within the joint capsule’s synovial fluid, which can lead to more inflammation and discomfort.
Causes of Cervical Osteoarthritis
Genetic predisposition may play a role in the development of cervical osteoarthritis.
Cervical osteoarthritis becomes more common as people age, so the natural wear and tear sustained by the facet joints over time is considered to be a major factor in its development. However, the medical community continues to study the issue and other factors also appear to play a role in the development of osteoarthritis, including:
- Genetics. Some evidence suggests that osteoarthritis can run in families, which would indicate some people are genetically predisposed to having cartilage that breaks down sooner.
- Injury. If the joint becomes injured, such as a tear in the cartilage and/or protective joint capsule, the joint can become more inflamed and cartilage can wear down sooner. Joint injuries can happen in various ways, such as from a fall or while participating in a sport.
- Occupation. Certain occupations, such as jobs that involve lots of repetitive motions or heavy lifting like construction, can put more stress on the cervical spine.
- Weight. People who are overweight tend to develop osteoarthritis sooner, including in the neck. More weight means more stress on the joints, but another possibility could be that people with excess weight might experience more damaging inflammation. 1 Cervical spondylosis. U.S. National Library of Medicine, MedlinePlus. https://medlineplus.gov/ency/article/000436.htm Reviewed April 2015.
Currently, the medical literature has limited data on whether or not smoking contributes to osteoarthritis in the spine. 2 Felson DT, Zhang Y. Smoking and osteoarthritis: a review of the evidence and its implications. Osteoarthritis and Cartilage. 2015; 23(3): 331-3. However, smoking has been linked to increasing neck pain in general.
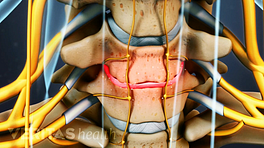
When Cervical Osteoarthritis Is Serious
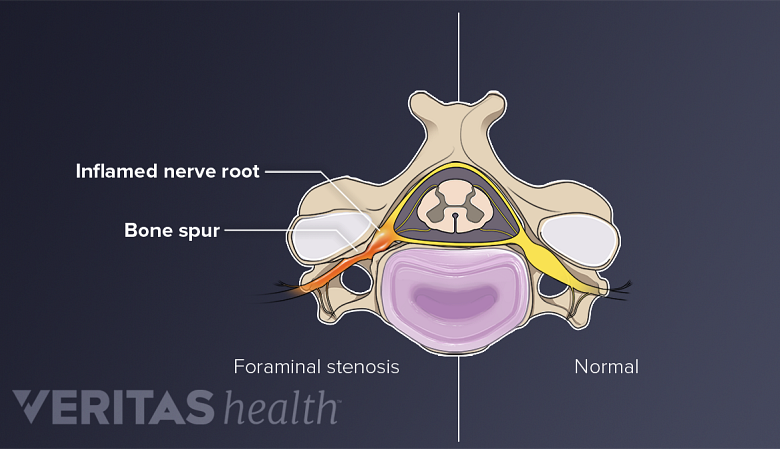
Cervical osteoarthritis with enlarged bone spurs can lead to a narrowing in the spinal canal, causing stenosis.
If cervical osteoarthritis becomes advanced and bone spurs become big enough, narrowing can start to occur in the spinal canal (cervical spinal stenosis) and/or the intervertebral foramen (foraminal stenosis).
When these spaces start to narrow, the spinal cord or a cervical nerve root can become compressed. Some serious symptoms that could result include difficulty gripping objects or even problems with walking or coordination. If the spinal cord or a nerve root is compressed for long enough without seeking medical attention, permanent damage can occur.
- 1 Cervical spondylosis. U.S. National Library of Medicine, MedlinePlus. https://medlineplus.gov/ency/article/000436.htm Reviewed April 2015.
- 2 Felson DT, Zhang Y. Smoking and osteoarthritis: a review of the evidence and its implications. Osteoarthritis and Cartilage. 2015; 23(3): 331-3.