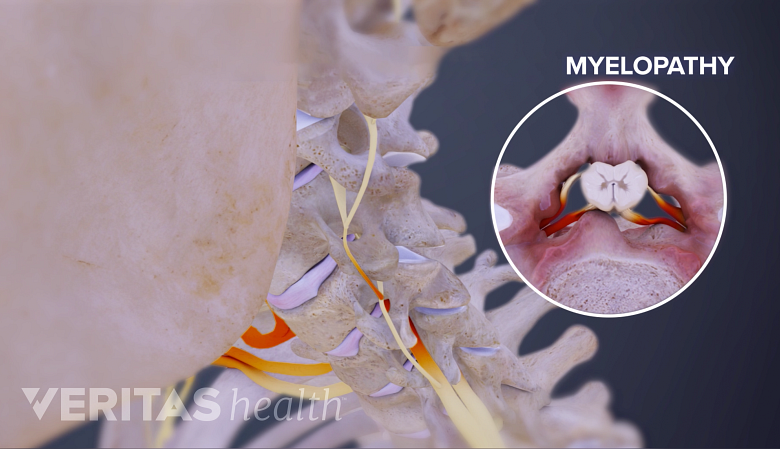
Cervical spinal stenosis, also called cervical stenosis, occurs when the neck’s protective spinal canal narrows due to degenerative changes or trauma. If the space within the spinal canal is reduced too much, neurologic deficits can result from spinal cord compression, a condition called myelopathy.
Conditions resulting from the natural degeneration of the spine can cause the spinal canal to narrow and compress nerve roots. Watch: Cervical Spinal Stenosis Video
This condition can result in a variety of serious symptoms anywhere in the body at or beneath the location of spinal cord impingement. Pain, numbness, weakness, and/or loss of coordination in one or more limbs or bodily functions may be the result.
Cervical stenosis with myelopathy is often referred to more generally as cervical spondylosis with myelopathy or cervical spondylotic myelopathy. The term spondylosis refers to degeneration of the spine, whereas stenosis specifically refers to the narrowing of the spinal canal that can happen as a part of spondylosis.
In This Article:
How Cervical Stenosis with Myelopathy is Caused
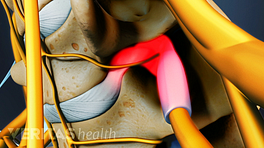
Spinal canal narrowing due to bone spurs or herniated discs causes cervical stenosis with myelopathy.
Everyone’s spine experiences some degeneration with age. Intervertebral discs, which provide cushioning between vertebral bones, naturally lose hydration over time and become flatter, and discs may bulge into the spinal canal. The joints in the back of the spine, called facet joints, also degenerate with time and become enlarged with changes from arthritis. The result of both of these types of degeneration is less room in the spinal canal, or spinal stenosis.
See How the Cervical Spine Changes With Age
Anything that narrows the spinal canal enough to compress the spinal cord—such as bone spurs, herniated discs, or swollen ligaments—can cause cervical stenosis with myelopathy. While spinal degeneration is typically a slow process that occurs from natural wear and tear over time, it can be accelerated by an injury to the spine.
See When Does the Neck’s Spinal Degeneration Become Painful?
The Course of Cervical Stenosis with Myelopathy
Cervical stenosis with myelopathy tends to get worse slowly over time, but there is some variation. Symptoms may remain stable for long periods or rapidly worsen.
Most cases of myelopathy will require an operation to relieve pressure on the spinal cord. In rare cases, symptoms of myelopathy are mild enough so that nonsurgical treatments are recommended. However, because of the risk of severe nerve damage, most surgeons will recommend an operation to relieve pressure on the spinal cord.
When Cervical Stenosis with Myelopathy is Serious
Severe weakness and numbness in the arms warrant immediate medical attention.
Early symptoms of cervical myelopathy include changes in coordination or fine motor skills of the arms, weakness/numbness in the arms or legs, or problems with balance. These should be taken seriously and checked out by a doctor. If treatment is not sought, the spinal cord can become more compressed and severe symptoms could result, such as paralysis in one or more limbs or other bodily functions shutting down.
See Spinal Cord Compression and Dysfunction from Cervical Stenosis