The term "stenosis" is derived from Greek and refers to the process of narrowing that constricts or "chokes" the spinal nerves. The cause of spinal stenosis in the lumbar spine (lower back) is commonly associated with degenerative changes, also known as spondylosis, that occur as a result of aging.
In This Article:
Causes of Lumbar Spinal Stenosis: Understanding Degenerative Changes and Nervous Tissue Compression
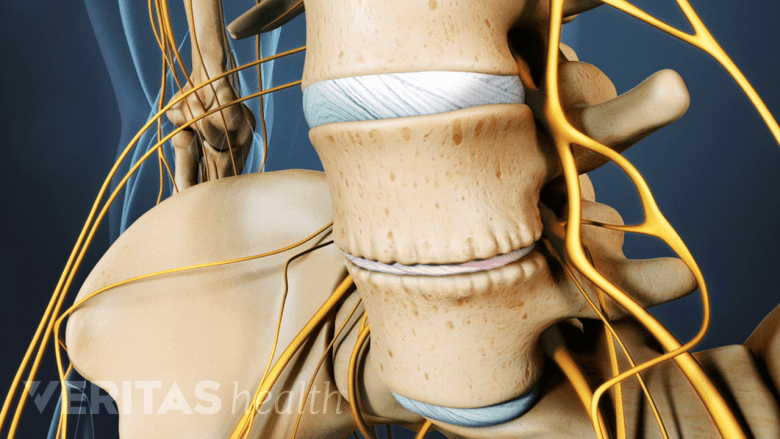
Lumbar spinal stenosis may occur when spinal discs are dehydrated and compresses the spinal nerves.
Most commonly, lumbar spinal stenosis occurs when spondylosis causes one or more of the following changes in the spine:
- Alterations within the facet joints, the small, stabilizing joints located between and behind vertebrae, which tend to get larger as they degenerate, compressing nearby spinal nerve roots.
- Dehydration of the spinal discs, resulting in the collapse of the inner soft, jelly-like material, decreasing the space available for the spinal nerves.
- Thickening of the spinal ligaments inside the vertebral canal, leading to compressive forces on the spinal cord and spinal nerves.
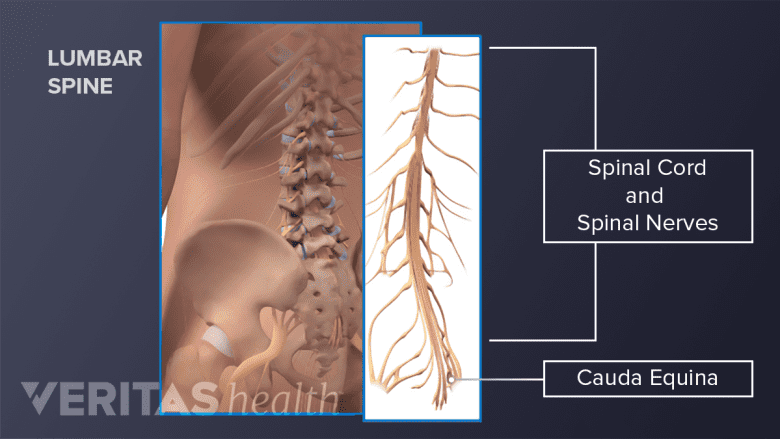
Stenosis in the lumbar spine may be diagnosed if degenerative changes have narrowed the bony openings of the spine and affected the nervous tissues, such as the spinal nerves, spinal cord, and/or the cauda equina.1Melancia JL, Francisco AF, Antunes JL. Spinal stenosis. In: Handbook of Clinical Neurology. Elsevier; 2014:541-549. doi:10.1016/b978-0-7020-4086-3.00035-7
Watch Lumbar Spine Anatomy Video
Understanding Lumbar Spinal Stenosis
Spinal stenosis in the lower back is more common in individuals over 60 years of age and typically affects the lower part of the lumbar spine—the L3 to L5 spinal levels.2Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010;24(2):253‐265. which causes symptoms to radiate into the leg.
In the initial stages, these changes often produce symptoms of pain and/or cramping in the legs, especially with activity. Over time, the pain may become more constant or severe. Additional symptoms, such as numbness and weakness may also occur.
Lumbar Spinal Stenosis: Types and Associated Symptoms
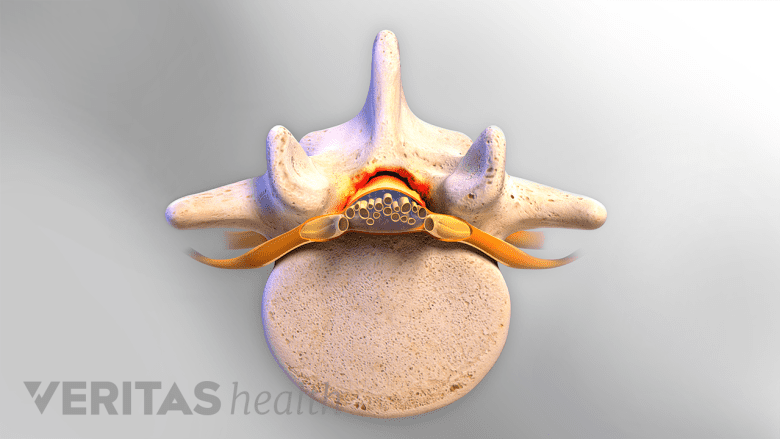
Central canal stenosis can affect the spinal cord.
There are 2 types of lumbar spinal stenosis:
1. Foraminal stenosis
2. Central canal stenosis
These types are described in detail below.
Foraminal stenosis: When spinal stenosis affects the spinal nerves as they run through the foramina (bony opening on each side of the lower spine), the condition is referred to as foraminal stenosis.
Central canal stenosis: Narrowing of the spine that encroaches on the spinal canal is also possible and is called central canal stenosis. Foraminal and central canal stenosis can occur at the same time, causing overlapping symptoms.3Patel J, Osburn I, Wanaselja A, Nobles R. Optimal treatment for lumbar spinal stenosis. Current Opinion in Anaesthesiology. 2017;30(5):598-603. doi:10.1097/aco.0000000000000495
When lumbar spinal stenosis occurs in conjunction with stenosis at a different level, such as in the cervical spine (neck) or thoracic spine (middle back), it is called tandem stenosis.
Depending on the location of the stenosis, various neural elements, such as the spinal nerve roots, spinal cord, and/or the cauda equina (nerves that descend from the spinal cord), may get compressed, leading to a combination of symptoms. These symptoms typically include (but are not limited to) pain, tingling, numbness, and/or weakness in the lower body, which presents as difficulty in walking.
Lumbar Spinal Stenosis: Common Signs and Symptoms
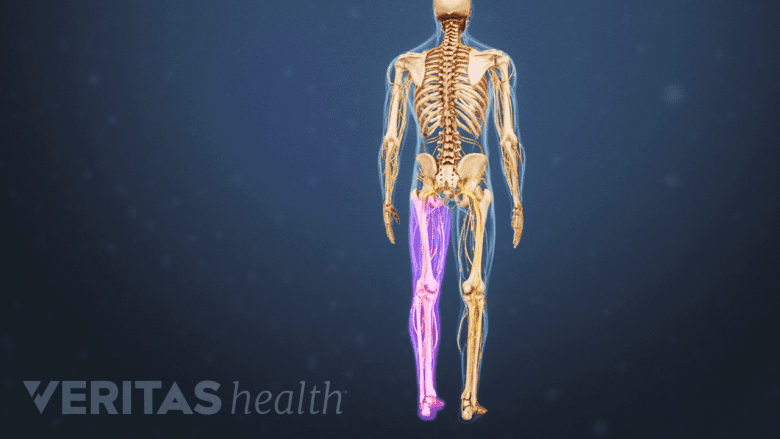
Nerve root compression results in leg pain, which travels down through the lower back and leg on one side.
The characteristic symptom of lumbar spinal stenosis is increased pain in the legs with walking (neurogenic claudication or pseudo claudication), which can markedly diminish one's activity level. People with lumbar spinal stenosis are typically comfortable at rest but cannot walk far without developing leg pain. Pain relief is achieved within 5 to 10 minutes when they sit down or lean forward.4Podnar S, Vodušek DB. Lower urinary tract dysfunction in patients with peripheral nervous system lesions. In: Neurology of Sexual and Bladder Disorders. Elsevier; 2015:203-224. doi:10.1016/b978-0-444-63247-0.00012-2 Spinal nerve root involvement may cause a more sharp, shooting type of pain in the leg.
The symptoms of lumbar spinal stenosis develop slowly. As the condition progresses, the symptoms may worsen and become quite debilitating. For each person, the severity and duration of lumbar stenosis symptoms are different and based on the affected neural tissue(s). Common symptoms may include one or more of the following:
- Leg pain: Nerve root compression or irritation that results in leg pain, which typically travels down from the lower back into the buttock and leg on one side—commonly called sciatica.
- Lumbar radiculopathy: Nerve root compression or irritation that results in tingling, weakness, and/or numbness that radiates from the lower back into the buttock and leg on one side.
- Neurogenic claudication: Spinal cord compression that causes a symmetrical pattern of pain affecting both legs while walking or standing for a long period of time. Neurologic deficits, such as loss of coordination, gait imbalance, numbness, and weakness affecting both legs may also occur.
For most people, symptoms of lumbar stenosis fluctuate, with some periods of more severe symptoms and some with fewer or none. The symptoms develop gradually and can lead to chronic pain and muscle weakness over time. It is also possible for lumbar spinal stenosis to be asymptomatic (not cause any symptoms).5Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716.,6Munakomi S, Foris LA, Varacallo M. Spinal Stenosis And Neurogenic Claudication. [Updated 2019 Sep 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430872/
Read more about Lumbar Spinal Stenosis Symptoms
Causes of Lumbar Spinal Stenosis
The majority of lumbar spinal stenosis diagnoses identify the cause as degenerative changes in the spine (spondylosis) due to aging.7Wu L, Cruz R. Lumbar Spinal Stenosis. [Updated 2019 Dec 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531493/ The condition may also be caused by trauma, metabolic conditions, infections, or prior spinal surgery.
Spinal stenosis may also be present at birth, called congenital spinal stenosis.1Melancia JL, Francisco AF, Antunes JL. Spinal stenosis. In: Handbook of Clinical Neurology. Elsevier; 2014:541-549. doi:10.1016/b978-0-7020-4086-3.00035-7
Progression of Lumbar Spinal Stenosis
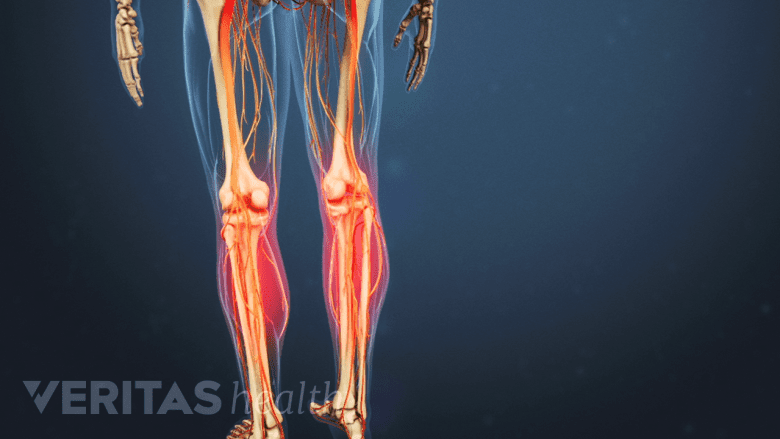
Cramping in the legs after a long walk is a classic symptom of lumbar spinal stenosis.
Often, a particular event or injury does not cause lumbar spinal stenosis—the condition develops over time. The risk of lumbar spinal stenosis increases with advancing age; the condition is more common in people over age 60 years.2Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010;24(2):253‐265. The presentation and progression of symptoms of this condition vary considerably. Early symptoms may include cramping or discomfort in the leg(s) after a long walk or a sensation of leg numbness or achiness after prolonged standing. In the later stages, the symptoms may progress into more severe leg pain that is exacerbated while walking.
Lumbar spinal stenosis typically does not have a standard course of development and may not necessarily get more severe with time. While it has not been definitively studied, small some studies have shown that the course of this condition is variable, even for patients with the same type of stenosis.8Minamide A, Yoshida M, Maio K. The natural clinical course of lumbar spinal stenosis: a longitudinal cohort study over a minimum of 10 years. J Orthop Sci. 2013;18(5):693‐698.
Over time, the symptoms may improve, worsen, or be intermittent with occasional flareups and/or activity-related pain.9Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. January 2016:h6234. doi:10.1136/bmj.h6234
When Lumbar Spinal Stenosis Is Serious
Compression of the cauda equina nerves warrants immediate medical attention.
While rare, it is possible for lumbar spinal stenosis to lead to serious complications. Immediate medical attention is warranted when the lumbar stenosis compresses the spinal cord and/or the cauda equina.
Signs and symptoms that indicate compression of these tissues typically include one or more of the following:
- Almost intolerably severe lower back pain
- Severe sharp, shooting, and burning pain in the leg(s)
- Progressive weakness in one or both legs
- Numbness of the inner thighs (saddle anesthesia) and/or around the anal region
- Urinary retention
- Loss of bowel and/or bladder control (either inability to retain or release)
These symptoms may indicate cauda equina syndrome10Berg EJ, Ashurst JV. Anatomy, Back, Cauda Equina. [Updated 2018 Dec 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513251/ (compression of the cauda equina nerves) or conus medullaris syndrome11Nene Y, Jilani TN. Neuroanatomy, Conus Medullaris. [Updated 2019 Aug 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545227/ (compression of the terminal part of the spinal cord). These syndromes need immediate medical intervention to preserve leg function.
Lumbar spinal stenosis can cause mild to serious symptoms, affecting daily life. While nonsurgical treatments are tried first, the patient may decide to have surgery if the symptoms are severe and cause significant dysfunction.
As with many spine conditions, health care professionals can advise on a range of nonsurgical and surgical treatments, and it is the patient’s choice to decide how to manage their condition.
Foundational elements of almost every lumbar stenosis treatment program will include medication, physical therapy, exercise, and weight management. More invasive treatments, such as an epidural steroid injection or surgery, may be considered if the symptoms worsen and interfere with the patient’s mobility and everyday life. Surgical treatment shows better improvement when the symptoms are severe.6Munakomi S, Foris LA, Varacallo M. Spinal Stenosis And Neurogenic Claudication. [Updated 2019 Sep 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430872/
Lumbar spinal stenosis is the most common indication for spinal surgery in patients over 65 years of age.5Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716.
- 1 Melancia JL, Francisco AF, Antunes JL. Spinal stenosis. In: Handbook of Clinical Neurology. Elsevier; 2014:541-549. doi:10.1016/b978-0-7020-4086-3.00035-7
- 2 Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010;24(2):253‐265. The presentation and progression of symptoms of this condition vary considerably. Early symptoms may include cramping or discomfort in the leg(s) after a long walk or a sensation of leg numbness or achiness after prolonged standing. In the later stages, the symptoms may progress into more severe leg pain that is exacerbated while walking.
- 3 Patel J, Osburn I, Wanaselja A, Nobles R. Optimal treatment for lumbar spinal stenosis. Current Opinion in Anaesthesiology. 2017;30(5):598-603. doi:10.1097/aco.0000000000000495
- 4 Podnar S, Vodušek DB. Lower urinary tract dysfunction in patients with peripheral nervous system lesions. In: Neurology of Sexual and Bladder Disorders. Elsevier; 2015:203-224. doi:10.1016/b978-0-444-63247-0.00012-2
- 5 Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716.
- 6 Munakomi S, Foris LA, Varacallo M. Spinal Stenosis And Neurogenic Claudication. [Updated 2019 Sep 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430872/
- 7 Wu L, Cruz R. Lumbar Spinal Stenosis. [Updated 2019 Dec 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531493/
- 8 Minamide A, Yoshida M, Maio K. The natural clinical course of lumbar spinal stenosis: a longitudinal cohort study over a minimum of 10 years. J Orthop Sci. 2013;18(5):693‐698.
- 9 Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. January 2016:h6234. doi:10.1136/bmj.h6234
- 10 Berg EJ, Ashurst JV. Anatomy, Back, Cauda Equina. [Updated 2018 Dec 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513251/
- 11 Nene Y, Jilani TN. Neuroanatomy, Conus Medullaris. [Updated 2019 Aug 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545227/

