Degenerative changes in the spinal tissues associated with aging result in the vast majority of lumbar spinal stenosis diagnoses. 1 Huang W, Zhou G, Zhang Y. Risk factors for ligamentum flavum hypertrophy in lumbar spinal stenosis patients from the Xinjiang Uygur Autonomous Region, China: protocol for a retrospective, single-center study. Clinical Trials in Orthopedic Disorders. 2017;2(1):11. doi:10.4103/2542-4157.201057 , 2 Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716. A comprehensive evaluation of the potential sources is important for an accurate diagnosis of this condition.
In This Article:
- Lumbar Spinal Stenosis
- Lumbar Spinal Stenosis Symptoms
- Lumbar Spinal Stenosis Causes and Diagnosis
- Lumbar Spinal Stenosis Treatment
- Lumbar Spinal Stenosis Surgery Options
- Lumbar Spinal Stenosis Video
The Primary Causes of Lumbar Spinal Stenosis
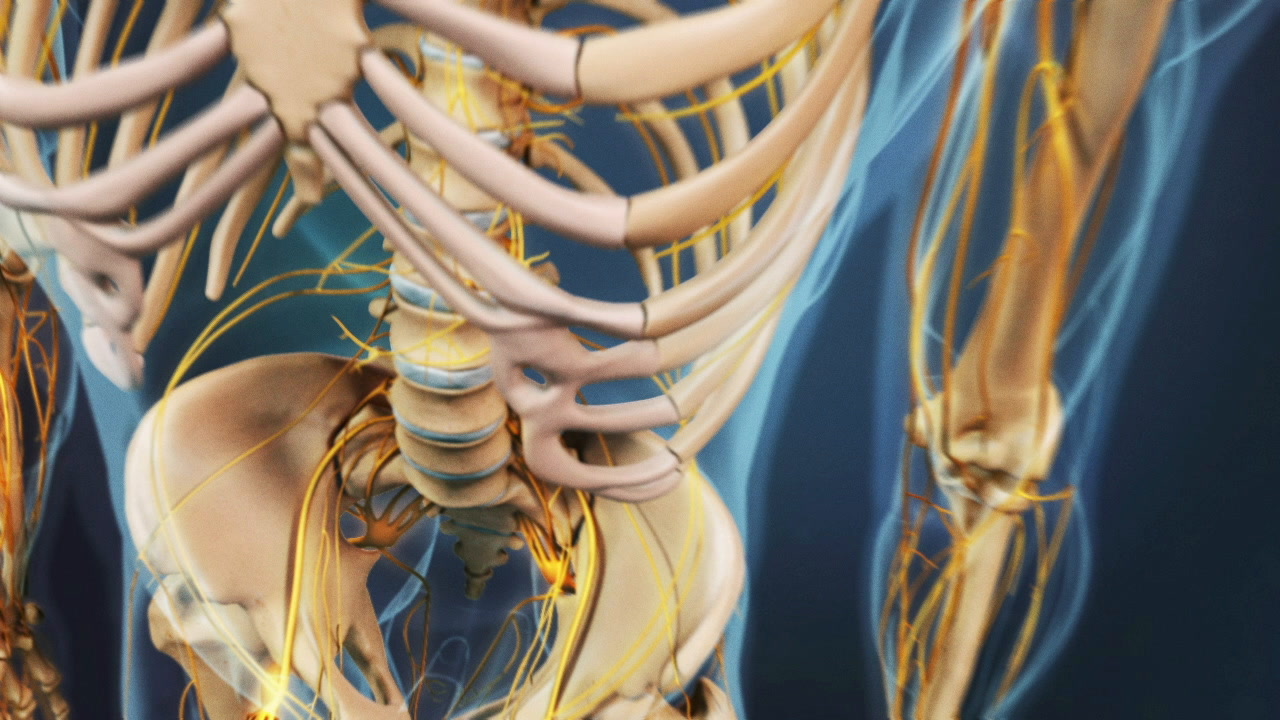
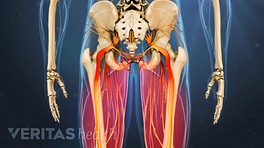
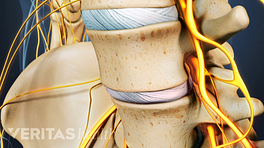
Aging-related degeneration may affect the spinal joints, ligaments, and/or the intervertebral discs, causing the following changes 2 Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716. :
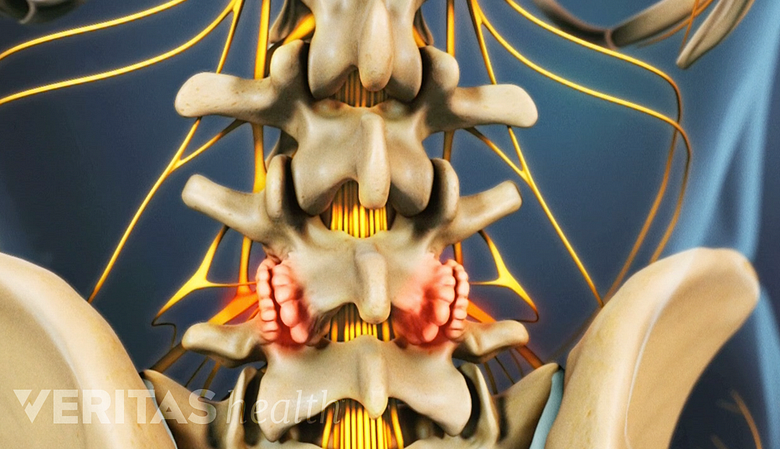
Hypertrophy of facet joints
Facet joint degeneration may lead to the development of bone spurs.
Arthritic degeneration may cause the facet joints to become arthritic and grow bone spurs (overgrown bone) that may impinge on spinal nerve roots and/or the spinal cord.
See Bone Spurs (Osteophytes) and Back Pain
Hypertrophy of ligamentum flavum
Thickening of the short bands of ligament that connects the inner surface of the spinal canal may compress the spinal cord.
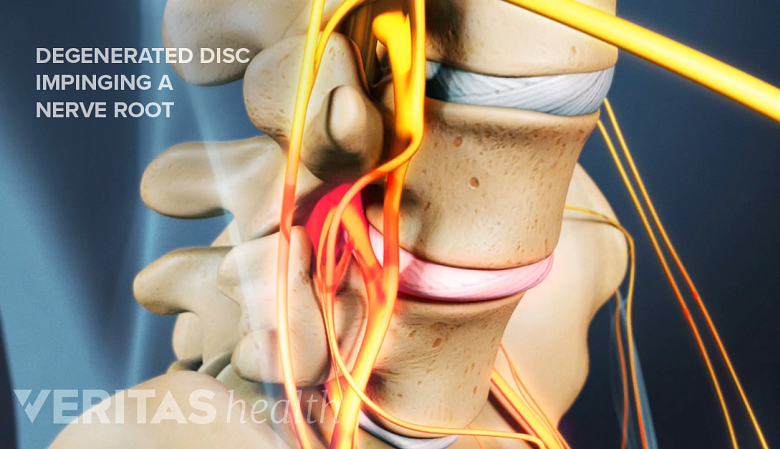
Degeneration of discs
Degenerated discs may compress the nearby spinal nerves.
Degeneration can cause a decrease in the height of intervertebral discs, reducing the disc space and narrowing the bony openings for spinal nerves (intervertebral foramen). Degeneration may also cause discs to herniate, compressing spinal nerve roots, and/or the spinal cord.
See What Is Degenerative Disc Disease?
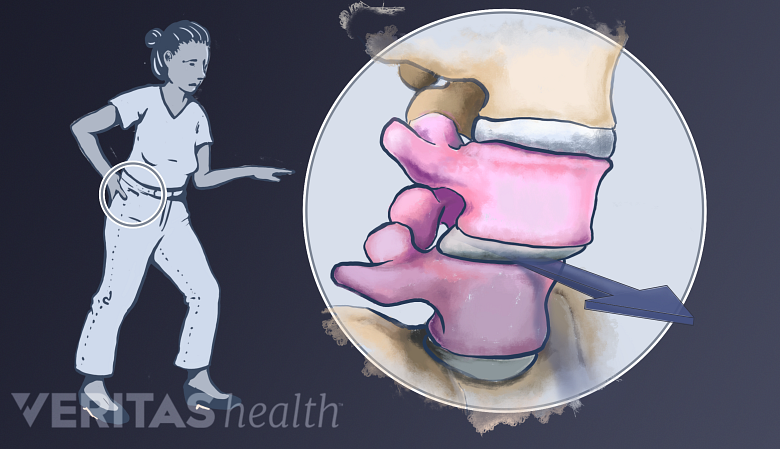
Degenerative spondylolisthesis
Age-related degeneration may cause spinal instability, leading to vertebral body slippage.
Age-related changes in the vertebrae may cause instability within the motion segment, resulting in slipping of a vertebral body over the one below it.
See Degenerative Spondylolisthesis
One condition may lead to the other, for example, a reduction in disc height may cause a bulging or buckling of the ligamentum flavum into the back of the spinal canal.
Less Common Causes of Lumbar Spinal Stenosis
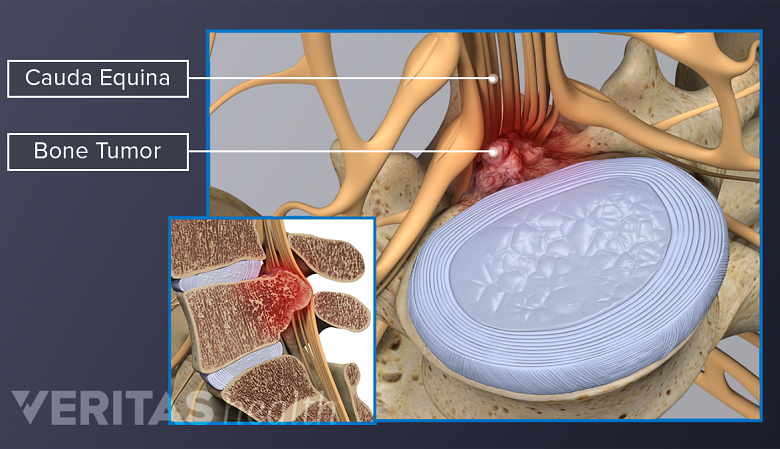
Rarely, tumors may compress the spinal cord or cauda equina.
Rarely, the following conditions may cause spinal stenosis in the lower back:
- Inherited or genetic, such as short vertebral pedicles (part of the vertebra that connects the vertebral body in front to the arch at the back) 2 Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716.
- Complications after lumbar surgery, such as laminectomy or lumbar fusion 2 Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716.
- Systemic conditions, such as Paget’s disease 2 Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716.
- Spinal growths, such as tumors, cysts, or abscess (collection of pus) in the lower spine
The risk of lumbar spinal stenosis typically increases with age. Risk factors also include genetic predisposition, being overweight, and occupations involving heavy physical labor. 1 Huang W, Zhou G, Zhang Y. Risk factors for ligamentum flavum hypertrophy in lumbar spinal stenosis patients from the Xinjiang Uygur Autonomous Region, China: protocol for a retrospective, single-center study. Clinical Trials in Orthopedic Disorders. 2017;2(1):11. doi:10.4103/2542-4157.201057
Diagnosis of Lumbar Spinal Stenosis
A doctor can diagnose stenosis in the lumbar spine based on specific clinical presentations and through medical imaging tests. Conducting a physical exam and reviewing the medical history helps a doctor determine the pattern of symptoms. Medical imaging tests help determine the location and severity of stenosis.
Physical exam and review of medical history
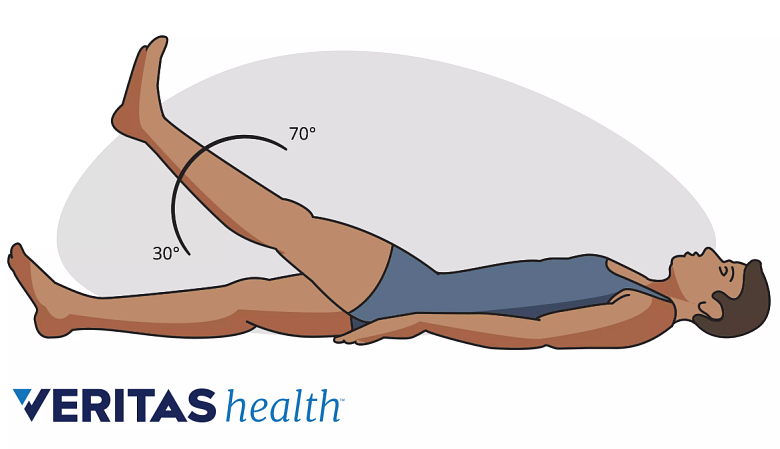
The straight leg raise test is performed to assess compression of sciatic nerve roots in the lumbar spine.
A doctor typically checks for pain, numbness, muscle reflexes, and nerve function in the legs. Specific elements of the physical exam will include one or more of the following:
- Romberg’s test. This test checks for spinal cord impairment. In this test, the patient stands without support, and with their eyes closed. A loss of balance indicates a positive test result and may signal spinal cord damage or severe lumbar nerve root compression between L4-L5 and/or L5-S1. 3 Dydyk AM, M Das J. Radicular Back Pain. [Updated 2020 Apr 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546593/
- Gait test. In this test, the doctor analyzes the walking pattern of the patient to check for a wide-based or steppage gait, or loss of balance while walking.
- Neurological tests. These tests include analyzing the leg’s muscle reflex to check for nerve root compression in the lower back.
- Straight leg raise test. This test aims to access sciatic nerve root compression in the lumbar and/or sacral spine. During this test, the patient lies on their back and the doctor gently lifts the patient’s leg. If pain is experienced during this maneuver, the test is considered positive.
During a physical exam, the doctor also reviews the medical history, which includes information about the onset and duration of symptoms, past surgeries, medications, and the presence of concomitant medical conditions.
Medical imaging tests for lumbar spinal stenosis
MRI is generally regarded as the most reliable test for diagnosing spinal stenosis.
Imaging tests may be helpful in locating the site and severity of lumbar spinal stenosis and include:
- Magnetic resonance imaging (MRI). An MRI is typically considered the gold standard test to identify spinal stenosis. MRI's are sensitive in identifying the size, shape, and associations between tissues of the spine and can provide details of important structures, such as degenerated discs. 4 Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. January 2016:h6234. doi:10.1136/bmj.h6234 , 5 Lee SY, Kim TH, Oh JK, Lee SJ, Park MS. Lumbar Stenosis: A Recent Update by Review of Literature. Asian Spine J. 2015;9(5):818–828. doi:10.4184/asj.2015.9.5.818
- Radiographs. Regular x-rays are useful in identifying fractures and defects of the vertebrae, alignment of the motion segment, loss of disc height, and bone spur formation. 4 Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. January 2016:h6234. doi:10.1136/bmj.h6234
- Computed tomography (CT) scans. A CT scan provides visualization of the spinal structures and may be done when an MRI is not available or possible.
- Myelography: A myelogram involves the injection of a radiographic dye into the spinal canal, which is followed by a CT scan. Myelograms are typically only performed in patients who cannot undergo an MRI or have had prior surgery.
It is important to understand that medical image findings may not always correlate with the symptoms. Up to 30% of adults older than 60 years may have imaging evidence of lumbar spinal stenosis with no symptoms. 2 Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716. A history of clinical symptoms along with imaging evidence is essential to diagnose symptomatic lumbar spinal stenosis. 4 Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. January 2016:h6234. doi:10.1136/bmj.h6234
Once lumbar spinal stenosis is identified as the cause of the patient’s symptoms, a definitive treatment plan can be formulated. Nonsurgical treatments are usually recommended for several weeks before surgical intervention is considered.
- 1 Huang W, Zhou G, Zhang Y. Risk factors for ligamentum flavum hypertrophy in lumbar spinal stenosis patients from the Xinjiang Uygur Autonomous Region, China: protocol for a retrospective, single-center study. Clinical Trials in Orthopedic Disorders. 2017;2(1):11. doi:10.4103/2542-4157.201057
- 2 Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716.
- 3 Dydyk AM, M Das J. Radicular Back Pain. [Updated 2020 Apr 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546593/
- 4 Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. January 2016:h6234. doi:10.1136/bmj.h6234
- 5 Lee SY, Kim TH, Oh JK, Lee SJ, Park MS. Lumbar Stenosis: A Recent Update by Review of Literature. Asian Spine J. 2015;9(5):818–828. doi:10.4184/asj.2015.9.5.818