There are a number of potential signs and symptoms of spinal stenosis. The specific signs and symptoms are mainly determined by the location and severity of the stenosis in the spine.
In This Article:
- What Is Spinal Stenosis?
- Types of Spinal Stenosis
- Spinal Stenosis Symptoms and Diagnosis
- Spinal Stenosis Treatment
- Spinal Stenosis Surgery
- Lumbar Spinal Stenosis Video
Common Spinal Stenosis Symptoms and Signs

Spinal stenosis can cause pain, numbness, and weakness in the back, neck, and limbs.
Some common symptoms and signs of spinal stenosis may include one or more of the following:
- Radicular pain that can radiate from the spine into an arm or leg, or less commonly into both arms or legs. This pain can range from a dull ache or tenderness to an electric-like pain or burning sensation.
- Radiculopathy, which involves neurological deficits stemming from spinal nerve root compression, such as tingling, numbness, or weakness that goes into an arm or leg.
- Myelopathy, which involves neurological deficits stemming from spinal cord compression, such as tingling, numbness, or weakness that goes into both arms and/or legs. Myelopathy could also involve dysfunction elsewhere in the body, such as problems with bladder/bowel control.
Cauda equina syndrome, which results in neurological deficits from compression of the cauda equina (spinal nerve roots that continue below the spinal cord). Numerous signs and symptoms may develop in the lower extremities, including saddle anesthesia and/or bowel/bladder incontinence. Cauda equina syndrome requires immediate medical attention to avoid permanent nerve damage.
While spinal stenosis is commonly associated with pain that radiates into the leg or arm, sometimes the pain is felt more locally within the spine, such as in the lower back or neck.
Onset of Spinal Stenosis Symptoms
Overall, spinal stenosis symptoms are often characterized as:
- Developing slowly over time, or slow onset
- Coming and going, as opposed to continuous pain
- Occurring during certain activities (such as walking or biking while holding the head upright with lumbar stenosis) and/or positions (such as standing upright with lumbar stenosis)
- Feeling relieved by rest (sitting or lying down) and/or any flexed (forward bending) position
While rare, it is also possible for spinal stenosis to present primarily as neurological deficits, such as numbness and/or weakness, rather than pain.
Spinal Stenosis Symptoms by Location
Depending on the site of occurrence, the signs and symptoms of spinal stenosis can differ. Common signs and symptoms for different locations are highlighted below.
Lumbar spinal stenosis
Spinal stenosis in the lumbar spine may compress a lumbar spinal nerve(s) and send pain, tingling, numbness, and/or weakness into the leg(s). If the cauda equina (spinal nerves that run down the lumbar spinal canal) becomes compressed, cauda equina syndrome may occur.
Cervical spinal stenosis
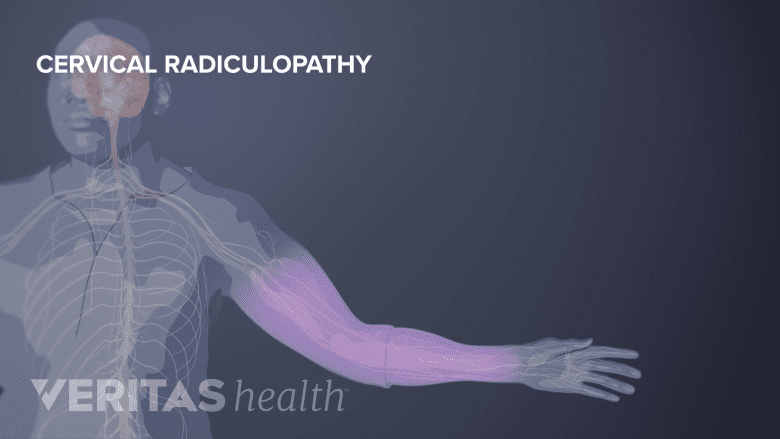
Cervical stenosis sends pain, weakness, and numbness down the arms.
Spinal stenosis in the cervical spine may compress a cervical spinal nerve(s) and send pain, tingling, numbness, and/or weakness into the arm(s). If the spinal cord becomes compressed, pain and/or neurological deficits may be experienced anywhere in the body beneath the level of compression, including the legs.
Thoracic spinal stenosis
Spinal stenosis in the thoracic spine may compress a thoracic spinal nerve(s) and send pain, tingling, numbness, and/or weakness into the chest or abdomen. If the spinal cord becomes compressed in the thoracic spine, pain and/or neurological deficits may be experienced at the level of compression (mid back) or below.
Spinal stenosis is most common in the lumbar spine and cervical spine. It rarely occurs in the thoracic spine. Spinal stenosis may also occur in multiple places, such as in both the cervical spine and lumbar spine (tandem stenosis).
Diagnosis of Spinal Stenosis
Getting an accurate diagnosis for spinal stenosis typically requires a 3-step process:
Patient history
A careful review of the patient’s medical history, including recent signs and symptoms, helps to narrow the list of possible causes.
Medical imaging

Medical imaging, such as an MRI, can be used to confirm or deny a diagnosis of stenosis.
While the patient history and physical examination may suggest spinal stenosis, the diagnosis must be confirmed with medical imaging. When imaging shows narrowing of the intervertebral foramen and/or vertebral foramen that corresponds with the patient’s symptoms, spinal stenosis is diagnosed. An MRI is the most common imaging used to diagnose spinal stenosis, but CT with myelography may be used in cases where MRI is not an option. It is also important to note that many people have spinal stenosis based on what is seen on medical imaging but have no symptoms and need no treatment.
Physical Examination
A medical professional observes and palpates (feels) the spine, such as along the neck or lower back. In addition to testing the spine’s range of motion, clinical tests may also be performed for leg and/or arm strength, reflexes, and sensation (tingling/numbness). Provocative tests may also be applied to see which movements or positions might cause nerve compression and pain to worsen. For example, Spurling’s test may be performed on the neck. This test involves rotating the head toward the symptomatic side, moving it into extension, and then gently applying pressure on top of the head to see if the pain is reproduced.
Other diagnostics that may be used include electrodiagnostic testing and diagnostic injections, which may help identify which specific spinal nerve is symptomatic.

