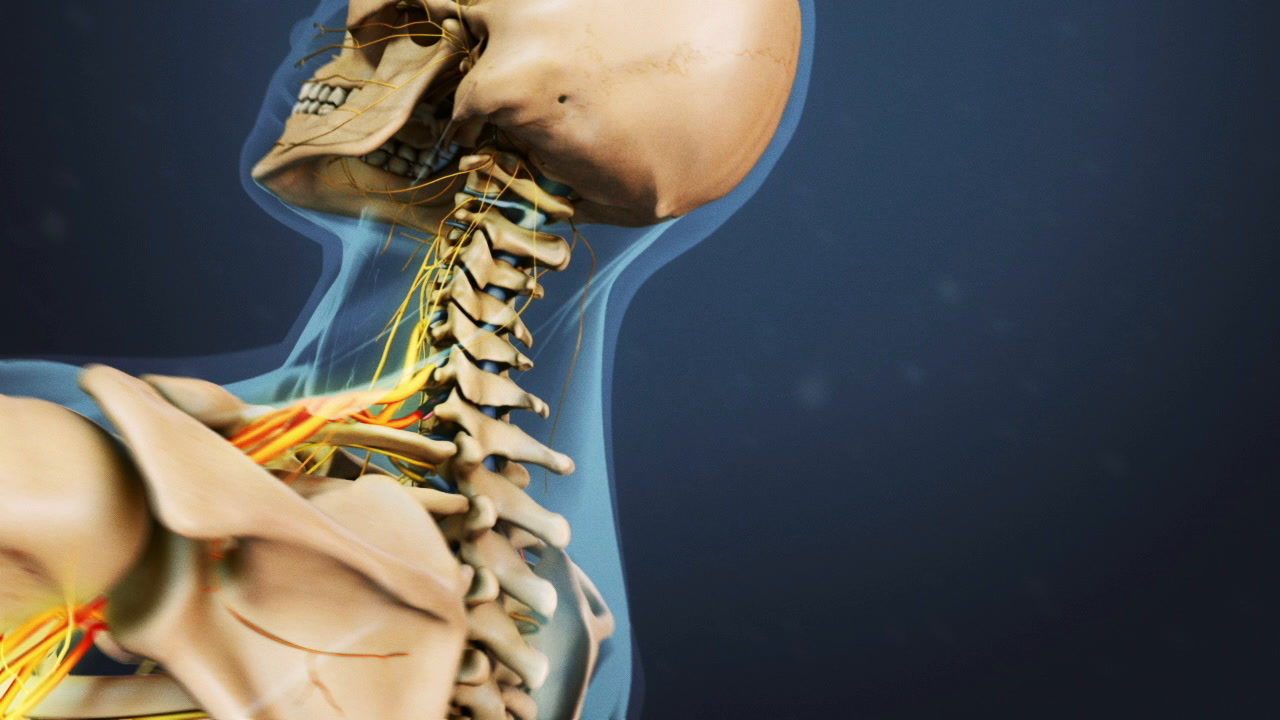
Surgery in the cervical spine may be recommended to treat problems in the neck, such as misalignment, compressed nerves, and/or spinal cord abnormalities.
The most common reasons for cervical spine surgery are to:
- Remove parts of the bone or disc that are causing nerve pain
- Fuse adjacent vertebrae together to create stability
- Widen the spinal canal to relieve spinal cord compression
- Remove tumors or masses
- Some combination of the above reasons
The most common type of neck surgery is ACDF, which is the acronym for anterior cervical discectomy and fusion.1Ahn Y. The Current State of Cervical Endoscopic Spine Surgery: an Updated Literature Review and Technical Considerations. Expert Rev Med Devices. 2020;17(12):1285-1292. doi:10.1080/17434440.2020.1853523
The C5-C6 and C6-C7 spinal motion segments are common levels in the neck to require surgical intervention.2Park DH, Ramakrishnan P, Cho TH, et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level. J Neurosurg Spine. 2007;7(3):336-340. doi:10.3171/SPI-07/09/336,3Kim HJ, Nemani VM, Piyaskulkaew C, Vargas SR, Riew KD. Cervical Radiculopathy: Incidence and Treatment of 1,420 Consecutive Cases. Asian Spine J. 2016;10(2):231-237. doi:10.4184/asj.2016.10.2.231
In This Article:
Goals of Cervical Spine Surgery
Cervical surgeries aim to relieve neck/arm pain caused by spinal cord or nerve root compression.
Neck surgery is usually done to relieve symptoms caused by one of two types of pathologies:
- Spinal cord compression in the neck, also called cervical spondylotic myelopathy
- Spinal nerve root compression in the neck, also called cervical radiculopathy
The specific surgical objectives are tailored for each patient based on the location and nature of the anatomic abnormality.
For example, surgery to treat nerve pain from cervical degenerative disc disease focuses on relieving pain and nerve pressure, while surgery to treat spinal cord compression focuses on restoring function and preventing further damage.
The goals of most cervical spine surgeries are to4American Academy of Orthopaedic Surgeons. Cervical Radiculopathy: Surgical Treatment Options. OrthoInfo. Accessed September 27, 2023. https://orthoinfo.aaos.org/en/treatment/cervical-radiculopathy-surgical-treatment-options:
- Alleviate neck and/or arm pain
- Maintain spinal stability
- Improve spine alignment
- Preserve neck mobility and range of motion
In some cases, cervical surgery is done to revise a previous failed surgery and achieve better outcomes.
Types of Cervical Spine Surgery
Cervical disc replacement surgery removes a damaged disc, replacing it with an artificial implant.
There are 3 types of neck surgery:
- Decompression: This technique is done to “decompress” the spinal cord or nerves in the neck by removing a piece of bone, disc, or other structure compressing the neural tissue.
- Fusion: This surgery corrects instability in the cervical spine through fusion, which sets up the process for a solid bony bridge to form between the vertebrae.
- Disc replacement: This surgery removes the entire damaged disc and replaces it with an artificial disc implant.
Decompression and fusion procedures are often combined in an ACDF surgery, where fusion is done alongside the decompression to prevent destabilization of the cervical spine. Spinal instrumentation (such as a small plate and screws) is used to add stability to the fused spinal construct.
Decompression and disc replacement surgeries preserve the spine’s natural motion, while fusion surgery immobilizes the spinal segment.
When Cervical Spine Surgery Is Recommended
Arm pain and numbness that persist beyond 6 months of non-surgical treatment may necessitate surgical management.
Common indications for neck surgery include:
- Persistent or recurrent arm pain and/or numbness unresponsive to non-surgical treatment for at least 6 months5Kang KC, Jang TS, Jung CH. Cervical Radiculopathy: Focus on Factors for Better Surgical Outcomes and Operative Techniques. Asian Spine J. 2022;16(6):995-1012. doi:10.31616/asj.2022.0445,6Yoon WW, Koch J. Herniated discs: when is surgery necessary?. EFORT Open Rev. 2021;6(6):526-530. Published 2021 Jun 28. doi:10.1302/2058-5241.6.210020,7Donnally III CJ, Hanna A, Odom CK. Cervical Myelopathy. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482312/
- Progressive neurological deficits, particularly definitive motor weakness5Kang KC, Jang TS, Jung CH. Cervical Radiculopathy: Focus on Factors for Better Surgical Outcomes and Operative Techniques. Asian Spine J. 2022;16(6):995-1012. doi:10.31616/asj.2022.0445
- Magnetic resonance imaging (MRI) or other imaging findings that correlate with and confirm the patient's signs and symptoms5Kang KC, Jang TS, Jung CH. Cervical Radiculopathy: Focus on Factors for Better Surgical Outcomes and Operative Techniques. Asian Spine J. 2022;16(6):995-1012. doi:10.31616/asj.2022.0445
Cervical spine surgery is generally elective, meaning that it is the patient's decision to have surgery or to continue with nonsurgical treatments.
Conditions such as spinal tumors, traumatic injury from a fall or motor vehicle accident, and/or acute injury to the spinal cord usually necessitate immediate medical attention and possible surgical intervention.
Conditions Treated with Cervical Spine Surgery
Cervical herniated discs are a common indication for neck surgery.
Neck surgery is recommended in the treatment of a number of traumatic, mechanical, and/or degenerative conditions, including:
- Cervical degenerative disc disease
- Cervical facet joint degeneration
- Cervical herniated discs
- Cervical stenosis with myelopathy
- Cervical spondylolisthesis
- Spondylosis
- Ligament ossification, such as ossified posterior longitudinal ligament (OPLL)
- Traumatic instability of the cervical spine
- Spinal tumors
The surgery is approached from the front (anterior approach) or back (posterior approach). In rare cases, a combined anterior-posterior approach is used.
In general, where possible, most surgeons favor an anterior approach.
Cervical Spine Surgery: Anterior Approach
A front approach provides direct access to the cervical disc and other anatomical structures in the front of the neck. Potential advantages of the anterior cervical approach include8Sugawara T. Anterior Cervical Spine Surgery for Degenerative Disease: A Review. Neurol Med Chir (Tokyo). 2015;55(7):540-546. doi:10.2176/nmc.ra.2014-0403:
- Direct visualization and access to anterior cervical pathology
- Minimal damage to neck muscles since no muscles attach to the midline front surface of the cervical vertebral body
An anterior cervical approach risks injuring delicate anatomical structures such as the recurrent laryngeal nerve, esophagus, and major blood vessels in the front of the neck.8Sugawara T. Anterior Cervical Spine Surgery for Degenerative Disease: A Review. Neurol Med Chir (Tokyo). 2015;55(7):540-546. doi:10.2176/nmc.ra.2014-0403
When an anterior cervical approach is considered
Good candidates for anterior cervical surgery typically include cases where8Sugawara T. Anterior Cervical Spine Surgery for Degenerative Disease: A Review. Neurol Med Chir (Tokyo). 2015;55(7):540-546. doi:10.2176/nmc.ra.2014-0403:
- The pathology is limited to 3 disc levels or less
- Spinal fusion and/or corpectomy (removal of the vertebra and disc) procedures are required
In general, patients with anterior cervical lesions such as bone spurs or disc herniations causing radiculopathy or myelopathy are considered for anterior surgery.8Sugawara T. Anterior Cervical Spine Surgery for Degenerative Disease: A Review. Neurol Med Chir (Tokyo). 2015;55(7):540-546. doi:10.2176/nmc.ra.2014-0403
Types of cervical spine surgery approached from the front
Common surgeries approached from the front of the neck include8Sugawara T. Anterior Cervical Spine Surgery for Degenerative Disease: A Review. Neurol Med Chir (Tokyo). 2015;55(7):540-546. doi:10.2176/nmc.ra.2014-0403:
- Anterior cervical discectomy with fusion (ACDF)
- Anterior cervical corpectomy with fusion (ACCF)
- Cervical artificial disc replacement
Research indicates that ACDF and cervical artificial disc replacement are the most widely performed surgeries for treating a range of cervical spine conditions.9Lukasiewicz AM, Basques BA, Bohl DD, Webb ML, Samuel AM, Grauer JN. Myelopathy is associated with increased all-cause morbidity and mortality following anterior cervical discectomy and fusion: a study of 5256 patients in American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP). Spine (Phila Pa 1976). 2015;40(7):443-449. doi:10.1097/BRS.0000000000000785,10Barbosa TP, Raposo AR, Cunha PD, et al. Rehabilitation after cervical and lumbar spine surgery. EFORT Open Rev. 2023;8(8):626-638. Published 2023 Aug 1. doi:10.1530/EOR-23-0015
Cervical Spine Surgery: Posterior Approach
The posterior approach in neck surgery enables direct visualization of the spinal canal and herniated discs.
Accessing the neck from the back allows the surgeon to directly visualize the spinal canal, spinal ligaments, and posterior disc herniation.
When a posterior cervical approach is considered
Surgical approach from the back of the neck is suited for treating:
- Posterior lesions, such as ligament ossification or thickened lamina, compressing the spinal cord or nerve roots8Sugawara T. Anterior Cervical Spine Surgery for Degenerative Disease: A Review. Neurol Med Chir (Tokyo). 2015;55(7):540-546. doi:10.2176/nmc.ra.2014-0403
- Pathology extending beyond 3 vertebral levels8Sugawara T. Anterior Cervical Spine Surgery for Degenerative Disease: A Review. Neurol Med Chir (Tokyo). 2015;55(7):540-546. doi:10.2176/nmc.ra.2014-0403
- Ossification of the posterior longitudinal ligament (OPLL) with widespread dural ossification8Sugawara T. Anterior Cervical Spine Surgery for Degenerative Disease: A Review. Neurol Med Chir (Tokyo). 2015;55(7):540-546. doi:10.2176/nmc.ra.2014-0403
- Extensive spinal stenosis that spans multiple levels or narrowing of the whole spinal canal11Hitchon PW, Woodroffe RW, Noeller JA, Helland L, Hramakova N, Nourski KV. Anterior and Posterior Approaches for Cervical Myelopathy: Clinical and Radiographic Outcomes. Spine (Phila Pa 1976). 2019;44(9):615-623. doi:10.1097/BRS.0000000000002912
The selection of a posterior approach is usually based on the surgeon’s preference and experience, along with the patient’s anatomic characteristics.12Zhang J, Liang Q, Qin D, et al. The anterior versus posterior approach for the treatment of ossification of the posterior longitudinal ligament in the cervical spine: A systematic review and meta-analysis. J Spinal Cord Med. 2021;44(3):340-349. doi:10.1080/10790268.2019.1692179
Types of cervical spine surgery approached from the back
Common neck surgeries approached from the back include:
- Posterior cervical decompression surgery
- Posterior cervical decompression and fusion
- Posterior cervical laminectomy
- Posterior cervical foraminotomy
- Posterior cervical laminoplasty
The posterior approach also enables circumferential decompression when combined with anterior surgery for severe OPLL and dural ossification.8Sugawara T. Anterior Cervical Spine Surgery for Degenerative Disease: A Review. Neurol Med Chir (Tokyo). 2015;55(7):540-546. doi:10.2176/nmc.ra.2014-0403
Sometimes, two surgeries are done at the same time, for example, when cervical laminotomy and foraminotomy are done together, the surgery is called posterior cervical laminoforaminotomy.
Cervical Spine Surgery Is Becoming More Routine
With technological advancements, many cervical surgeries are now performed through minimally invasive techniques.
These techniques involve smaller incisions and less tissue disruption. When minimally invasive techniques are used, the surgery is typically associated with:
- Shorter hospital stays
- Less post-surgical pain
- Less blood loss
- Faster recovery
Additionally, there is a greater chance of surgery being performed on an outpatient basis, with patients returning home on the same day as surgery.
- 1 Ahn Y. The Current State of Cervical Endoscopic Spine Surgery: an Updated Literature Review and Technical Considerations. Expert Rev Med Devices. 2020;17(12):1285-1292. doi:10.1080/17434440.2020.1853523
- 2 Park DH, Ramakrishnan P, Cho TH, et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level. J Neurosurg Spine. 2007;7(3):336-340. doi:10.3171/SPI-07/09/336
- 3 Kim HJ, Nemani VM, Piyaskulkaew C, Vargas SR, Riew KD. Cervical Radiculopathy: Incidence and Treatment of 1,420 Consecutive Cases. Asian Spine J. 2016;10(2):231-237. doi:10.4184/asj.2016.10.2.231
- 4 American Academy of Orthopaedic Surgeons. Cervical Radiculopathy: Surgical Treatment Options. OrthoInfo. Accessed September 27, 2023. https://orthoinfo.aaos.org/en/treatment/cervical-radiculopathy-surgical-treatment-options
- 5 Kang KC, Jang TS, Jung CH. Cervical Radiculopathy: Focus on Factors for Better Surgical Outcomes and Operative Techniques. Asian Spine J. 2022;16(6):995-1012. doi:10.31616/asj.2022.0445
- 6 Yoon WW, Koch J. Herniated discs: when is surgery necessary?. EFORT Open Rev. 2021;6(6):526-530. Published 2021 Jun 28. doi:10.1302/2058-5241.6.210020
- 7 Donnally III CJ, Hanna A, Odom CK. Cervical Myelopathy. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482312/
- 8 Sugawara T. Anterior Cervical Spine Surgery for Degenerative Disease: A Review. Neurol Med Chir (Tokyo). 2015;55(7):540-546. doi:10.2176/nmc.ra.2014-0403
- 9 Lukasiewicz AM, Basques BA, Bohl DD, Webb ML, Samuel AM, Grauer JN. Myelopathy is associated with increased all-cause morbidity and mortality following anterior cervical discectomy and fusion: a study of 5256 patients in American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP). Spine (Phila Pa 1976). 2015;40(7):443-449. doi:10.1097/BRS.0000000000000785
- 10 Barbosa TP, Raposo AR, Cunha PD, et al. Rehabilitation after cervical and lumbar spine surgery. EFORT Open Rev. 2023;8(8):626-638. Published 2023 Aug 1. doi:10.1530/EOR-23-0015
- 11 Hitchon PW, Woodroffe RW, Noeller JA, Helland L, Hramakova N, Nourski KV. Anterior and Posterior Approaches for Cervical Myelopathy: Clinical and Radiographic Outcomes. Spine (Phila Pa 1976). 2019;44(9):615-623. doi:10.1097/BRS.0000000000002912
- 12 Zhang J, Liang Q, Qin D, et al. The anterior versus posterior approach for the treatment of ossification of the posterior longitudinal ligament in the cervical spine: A systematic review and meta-analysis. J Spinal Cord Med. 2021;44(3):340-349. doi:10.1080/10790268.2019.1692179