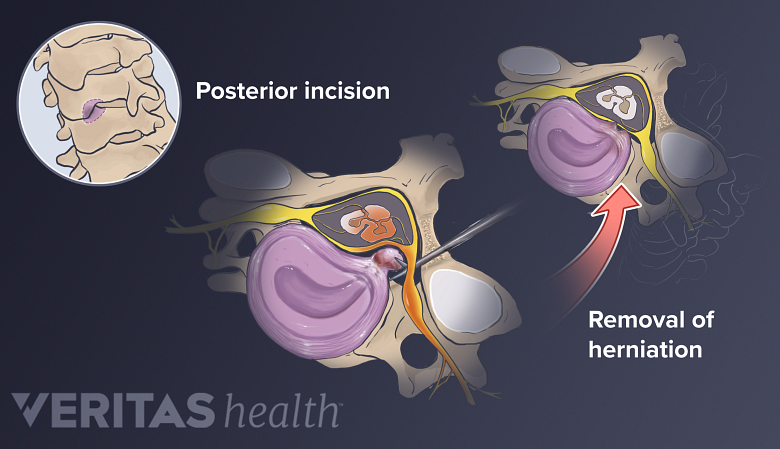
Some spine surgeons may prefer the posterior approach (from the back of the neck) for a cervical discectomy. This approach is often considered for large soft disc herniations that are lateral to (to the side of) the spinal cord.
See Outpatient Posterior Cervical Foraminotomy and Discectomy
Posterior Discectomy Advantages and Disadvantages
- The principal advantage of the posterior approach is that a spine fusion does not need to be done after removing the disc.
- The principal disadvantage is that the disc space cannot be jacked open with a bone graft to give more space to the nerve root as it exits the spine. Also, since the posterior approach leaves most of the disc in place, there is a small chance (3% to 5%) that a disc herniation may recur in the future.
What Occurs During Posterior Cervical Decompression?
The general procedure for the posterior cervical decompression (microdiscectomy) surgery includes the:
- Surgical approach.
- A small incision is made in the midline of the back of the neck.
- The para-spinal muscles are elevated off the spinal level that is to be approached.
- Disc removal.
- An x-ray is done to confirm that the surgeon is at the correct level of the spine.
- A high-speed burr is used to remove some of the facet joint, and the nerve root is then identified under the facet joint.
- An operating microscope is then used for better visualization.
- The disc will be directly under the nerve root, which needs to be gently mobilized (moved to the side) to free up the disc herniation.
- There is usually a plexus (network) of veins over the disc that can obstruct visualization if they bleed.
Posterior Cervical Discectomy Risks and Complications
Possible risks and complications of a posterior approach for cervical discectomy include:
- Nerve root damage
- Spinal cord damage
- Dural leak
- Infection
- Bleeding
- Continued pain
- Recurrent disc herniation.
In general, however, complications are rare.
In This Article:
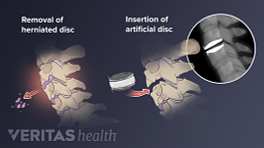
Posterior Versus Anterior Cervical Discectomy
The major advantage of approaching a cervical disc herniation through a posterior approach is that a fusion need not be performed. This preserves the normal motion of the cervical spine, and may provide for a shorter healing time.
See Cervical Herniated Disc Symptoms and Treatment Options
Although avoiding a fusion may sound desirable, the posterior approach has many disadvantages.
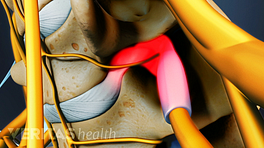
- Because the spinal cord is in the way, visualization of the disc space is limited, and typically only a disc herniation that is lateral (off to the side of the spine) can be approached.
- Also, by not doing a fusion from the anterior, the disc space is not distracted and the associated collapse that happens with a disc herniation can continue and place pressure on the nerve in the foramen (where the nerve exits the spine).
- Lastly, since the disc is not removed completely, it can re-herniate in the future.
In general, most surgeons prefer approaching the cervical spine from the anterior when possible because it is:
- A more reliable and definitive procedure
- Generally less demanding technically than a posterior approach.