There has been a significant increase in the number of spine surgery procedures that are now performed on an outpatient basis, meaning that the patient goes home the same day as the surgery and does not stay overnight in the hospital.
Learn more: What to Expect from Spine Surgery for Low Back Pain
In the past decade, this shift toward performing spine surgery in an outpatient setting has been dramatic. Thirty years ago, almost all surgeries were performed at a hospital on people who had been admitted as patients.
Over time, however, techniques have evolved, and safety concerns have been addressed. Now, health experts predict that 50 percent of all spine surgeries will be performed on an outpatient basis within the next five years. 1 Best MJ, Buller LT, Eismont FJ. National Trends in Ambulatory Surgery for Intervertebral Disc Disorders and Spinal Stenosis: A 12-year Analysis of the National Surveys of Ambulatory Surgery. Spine (Phila Pa 1976). 2015;40(21):1703-11. , 2 Baird EO, Egorova NN, McAnany SJ, Qureshi SA, Hecht AC, Cho SK. National trends in outpatient surgical treatment of degenerative cervical spine disease. Global Spine J. 2014;4(3):143-50. Epub 2014 Jul 14.
In This Article:
- Outpatient Spine Surgery Considerations
- Lumbar Discectomy Outpatient Spine Surgery
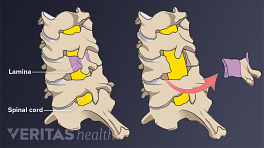
- Outpatient Lumbar Laminectomy or Laminotomy
- Outpatient Posterior Cervical Foraminotomy and Discectomy
- Outpatient Anterior Cervical Discectomy and Fusion (ACDF)
- Outpatient Lumbar Fusion
- Pain Management After Outpatient Spine Surgery
Potential Benefits of Outpatient Spine Surgery
There are several potential benefits of outpatient surgery, for example:
- Many patients find recovering at home is a more comfortable and satisfying experience
- The cost is reduced, as overnight stays in the hospital is a significant expense. This factor becomes more important depending on the patient's copay and insurance coverage
- The chance of infection is typically lower at home than at a hospital
Supporting this trend toward more outpatient surgeries is the growth of Ambulatory Surgery Centers (ASCs), which are set up and organized around surgeries that are done on an outpatient basis. Some ASCs, for example, have a type of concierge service, encompassing services such as transportation from the ASC to the patient's home or lodging, visiting nurses for followup care, and more.
Ideal Candidates for Outpatient Spinal Surgery
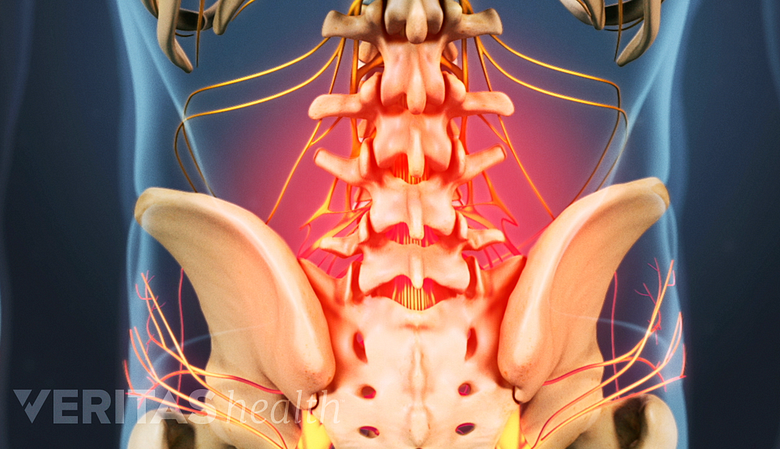
Patients unresponsive to nonsurgical treatment may be considered for microdiscectomy procedures.
Identifying people who are good candidates for outpatient surgery involves many factors. Most basically, the cause of the condition would be well defined, and the patient would have seen no improvement despite a reasonable amount of nonsurgical care.
If those conditions are met, the ideal candidate:
- Has no other medical conditions
- Is of normal weight (body mass index, or BMI, less than 35)
- Has sufficient family or social support at home
- Has a realistic expectation of some pain and discomfort despite reasonable pain-relief strategies
Not everyone is this ideal candidate, and each additional risk factor must be weighed before offering outpatient spine surgery.
See Spine Fusion Risks and Complications and Potential Risks and Complications of ACDF Surgery
This article details which spine surgery procedures are likely to be best for outpatient surgery and what considerations affect the choice of inpatient versus outpatient surgery.
- 1 Best MJ, Buller LT, Eismont FJ. National Trends in Ambulatory Surgery for Intervertebral Disc Disorders and Spinal Stenosis: A 12-year Analysis of the National Surveys of Ambulatory Surgery. Spine (Phila Pa 1976). 2015;40(21):1703-11.
- 2 Baird EO, Egorova NN, McAnany SJ, Qureshi SA, Hecht AC, Cho SK. National trends in outpatient surgical treatment of degenerative cervical spine disease. Global Spine J. 2014;4(3):143-50. Epub 2014 Jul 14.