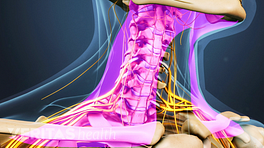
For most people about to have ACDF surgery, digestive health is the last thing on the mind. Once the surgery is over, priorities can quickly change during the recovery process and constipation may become one of the most inconvenient and troublesome symptoms.
See ACDF Surgery Postoperative Care
Constipation is typically diagnosed when a bowel movement has not occurred for at least three days. Symptoms that may accompany constipation include a painful, sharp, or bloated feeling in the stomach, nausea, and/or vomiting.
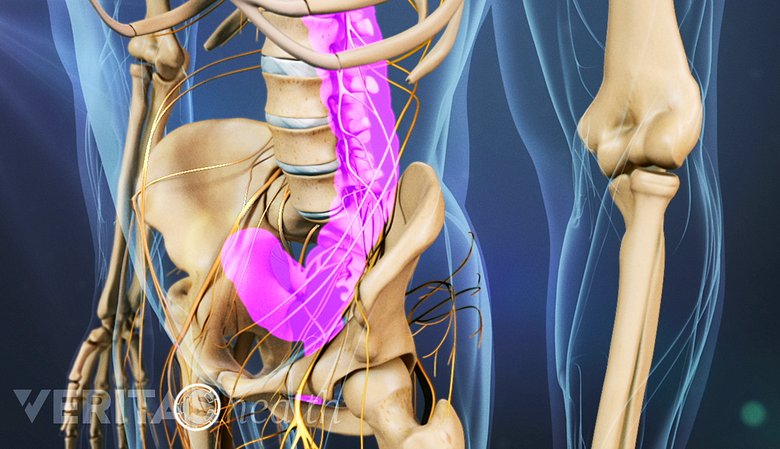
Several factors can lead to constipation in the days or weeks following ACDF, including a lack of exercise, poor diet, and the use of opioid pain medications.
Post-surgical constipation is one of the most inconvenient and troublesome symptoms.
In This Article:
- What to Expect After ACDF Surgery
- After ACDF: Trouble with Swallowing
- After ACDF: Trouble with Speaking
- After ACDF: Managing Mental Health
- After ACDF: How to Prevent or Manage Constipation
Steps to Prevent Constipation
Preventing constipation is much easier and more comfortable than having to treat it. If constipation develops while recovering from ACDF, it tends to be a more moderate or severe case rather than mild.
See Preventing Constipation After Back Surgery
Some tips to reduce the risk of developing constipation include:
- Get regular exercise. Finding the energy and motivation to exercise may be hard while recovering from an ACDF. However, if cleared by the doctor, walking every day is recommended to help promote healing and other health benefits, including regular bowel movements. Care should still be taken to avoid strenuous activities and/or overexertion, but too much rest and sitting is also not advised.
- Stay hydrated. Drinking enough water and other liquids can help avoid constipation caused by dehydration. According to the CDC, most adults can get enough liquids by having a beverage with each meal and also when thirsty. 1 Water and nutrition. Centers for Disease Control and Prevention Web site. Published October 5, 2016. Accessed August 9, 2016. Many foods also have a high water content, such as fruits and vegetables. As a rule of thumb, drinking at least 40 ounces of liquids (five 8-ounce glasses) per day in addition to a healthy diet is enough to stay hydrated.
- Eat plenty of fiber. The USDA recommends 14g of dietary fiber for every 1,000 calories consumed. 2 2015–2020 Dietary Guidelines for Americans. 8th Edition. U.S. Department of Health and Human Services and U.S. Department of Agriculture. December 2015. Having fruits, vegetables, and whole grains with each meal can help. Some foods especially high in fiber include peas, lentils, beans, artichokes, broccoli, raspberries, and pears. For a patient who might still have a sore throat or struggle with swallowing, a blender may need to be used. Also, avoid eating too much fiber as that can also cause problems, including constipation.
- Avoid or limit fatty and processed foods. These foods are hard to digest and contribute to hardening of stools and constipation.
- Take a fiber laxative. This type of laxative helps provide better bowel movement by bulking up the stool and enabling more water to stay in the colon. Some ACDF patients start taking fiber laxatives shortly after surgery as a preventive measure. A couple examples include Citrucel and Metamucil.
- Monitor pain medication use. Some pain medications, especially opioids, can severely slow the colon’s ability to move stool through the system. If pain has reduced to a more tolerable level, sometimes it is advised to switch to a weaker pain reliever, such as acetaminophen (Tylenol), in order to reduce the risk of having constipation. More importantly, the risk of developing constipation is a good reason to avoid taking the opioids more frequently than prescribed.
How to Manage Constipation During ACDF Recovery
If constipation develops while recovering from ACDF surgery, part of the treatment plan is likely to be the same as the preventive measures: drink plenty of liquids, incorporate high-fiber foods into the diet, and increase activity or exercise levels if feasible.
Other treatment options may include:
- Switch pain medication. If the pain medication is suspected of making constipation symptoms worse, the doctor may try a different one.
- Stimulant laxatives. These laxatives help stimulate muscle contractions to move stool through the colon. If fiber laxatives have not provided relief, stimulant laxatives may be recommended on a short-term basis. Some examples include Dulcolax, Ex-Lax, and milk of magnesia.
- Stool softeners. For stools that are too hard, a stool softener can help mix in moisture to soften and more easily move them through the colon. Some examples include Colace (Docusate) and Senna.
- Suppositories or enemas. Rather than being taken orally, these treatment options are placed in the rectum. A suppository is a small package filled with medicine that acts as a laxative and stool softener, whereas an enema typically injects saline liquid into the colon to stimulate bowel movement. If a suppository or enema does not work the first time, a doctor should be consulted.
This is not a full list of treatment options for constipation.
When to See a Doctor
If self-care does not alleviate constipation or if other worrisome symptoms are present, such as stomach pain or blood in the stool, seek medical attention. Untreated constipation could lead to hemorrhoids or other serious problems.
- 1 Water and nutrition. Centers for Disease Control and Prevention Web site. Published October 5, 2016. Accessed August 9, 2016.
- 2 2015–2020 Dietary Guidelines for Americans. 8th Edition. U.S. Department of Health and Human Services and U.S. Department of Agriculture. December 2015.