Nerves in the leg may become inflamed, compressed, or degenerated as a result of mechanical or chemical irritants. Nerves may also become damaged due to associated conditions such as diabetes or nutritional deficiencies. Depending on the cause of nerve damage, the specific leg symptoms may differ.
Nerve pain is typically described as sharp, shooting, electric-like, or searing pain. It may also produce a sensation of hot or warm water running down the thigh and/or leg. In some individuals, a dull ache may occur. The pain may be intermittent or constant.
See What You Need to Know About Sciatica
The most common types of nerve pain in the leg are described below.
In This Article:
Radiculopathy
The medical term for leg pain that originates from a problem in the nerve roots of the lumbar and/or sacral spine is radiculopathy (the lay term is sciatica). This pain may be caused when the nerve roots are inflamed, irritated, or compressed.1Alexander CE, Varacallo M. Lumbosacral Radiculopathy. [Updated 2019 Mar 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430837/ The characteristics of this pain depend on the specific nerve root(s) affected.
Research indicates 95% of radiculopathy in the lumbosacral spine occurs at the L4-L5 and L5-S1 levels. The pain from these nerve roots is characterized by2Wright R, Inbody SB. Radiculopathy and Degenerative Spine Disease. In: Neurology Secrets. Elsevier; 2010:121-130. doi:10.1016/b978-0-323-05712-7.00007-6:
- Pain that originates in the lower back or buttock and travels down the thigh, calf, and foot.
- Numbness in the calf, foot, and/or toes.
- Weakness in the hip, thigh, and/or foot muscles.
Depending on the individual, additional sensations may occur, such as a feeling of pins-and-needles in the leg, warm water running down the thigh, or the foot immersed in hot water. Radiculopathy typically affects one leg.
Peripheral Neuropathy
Leg pain and related symptoms could be the result of damage to a peripheral nerve.
Damage to one or more nerves in the peripheral nervous system (outside the brain and spinal cord) is called peripheral neuropathy. This form of neuropathy in the leg most commonly occurs due to diabetes.3Harati Y, Kwan J, Smyth S. Peripheral Neuropathies and Motor Neuron Diseases. In: Neurology Secrets. Elsevier; 2010:97-120. doi:10.1016/b978-0-323-05712-7.00006-4,4Callaghan BC, Price RS, Feldman EL. Distal Symmetric Polyneuropathy: A Review. JAMA. 2015;314(20):2172–2181. doi:10.1001/jama.2015.13611 Diabetic peripheral neuropathy commonly causes:
- Pain that originates in the toes and gradually spreads toward the knee (also called stocking-glove pattern; the action of putting on a stocking)
- Numbness in the legs and feet
- Weakness in the toes and ankles during the later stages of the condition
Peripheral neuropathy pain typically affects both legs.
See All About Neuropathy And Chronic Back Pain
Lumbosacral Radiculoplexus Neuropathy
This condition occurs due to inflammation of small blood vessels in the legs leading to reduced blood supply to the nerves, resulting in nerve damage. This condition is commonly seen in diabetic individuals and may also be caused by other issues. Common symptoms include5Ng PS, Dyck PJ, Laughlin RS, Thapa P, Pinto MV, Dyck PJB. Lumbosacral radiculoplexus neuropathy. Neurology. February 2019:10.1212/WNL.0000000000007020. doi:10.1212/wnl.0000000000007020:
- Pain that usually begins in a specific location, such as the buttock, hip, thigh, leg, or foot and gradually spreads to other areas of the leg
- Numbness and a prickling feeling in the affected areas
- Weakness in the leg muscles
- Loss of balance, which may cause falls
Typically, several nerves are affected together. The condition may develop in one leg and over time involve both legs.5Ng PS, Dyck PJ, Laughlin RS, Thapa P, Pinto MV, Dyck PJB. Lumbosacral radiculoplexus neuropathy. Neurology. February 2019:10.1212/WNL.0000000000007020. doi:10.1212/wnl.0000000000007020
Peroneal Neuropathy

Foot drop is characterized by difficulty or inability to walk on the heels of the feet.
Compression of the peroneal nerve near the knee may cause symptoms in the leg. Typical symptoms include6Poage C, Roth C, Scott B. Peroneal Nerve Palsy. Journal of the American Academy of Orthopaedic Surgeons. 2016;24(1):1-10. doi:10.5435/jaaos-d-14-00420:
- Foot drop, characterized by the inability to lift the foot, or a catch in the toes while walking
- Numbness along the side of the leg, the upper part of the foot, and/or the first toe web space
Pain is not a typical feature of this condition but may be present when peroneal neuropathy occurs as a result of trauma.
Meralgia Paresthetica
Compression of the lateral femoral cutaneous nerve in the thigh may cause a condition called meralgia paresthetica. Symptoms typically include7Cheatham SW, Kolber MJ, Salamh PA. Meralgia paresthetica: a review of the literature. Int J Sports Phys Ther. 2013;8(6):883-93.:
- Burning or achy pain in the outer side and/or front of the thigh
- Coldness in the affected areas
- Buzzing or vibrations (such as from a cell phone) in the thigh region
Meralgia paresthetica pain typically increases while standing or walking and alleviates while sitting.
Tarsal Tunnel Syndrome
Dysfunction of the tibial nerve due to nerve compression within the foot’s tarsal tunnel causes this syndrome. Common symptoms include8Kiel J, Kaiser K. Tarsal Tunnel Syndrome. [Updated 2019 Feb 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK513273/:
- Sharp, shooting pain in the inner ankle joint and along the sole of the foot
- Numbness in the sole of the foot
- Tingling and/or burning sensation in the foot
The symptoms typically worsen at night, with walking or standing, and/or after physical activity; and get better with rest.
Neurogenic Claudication
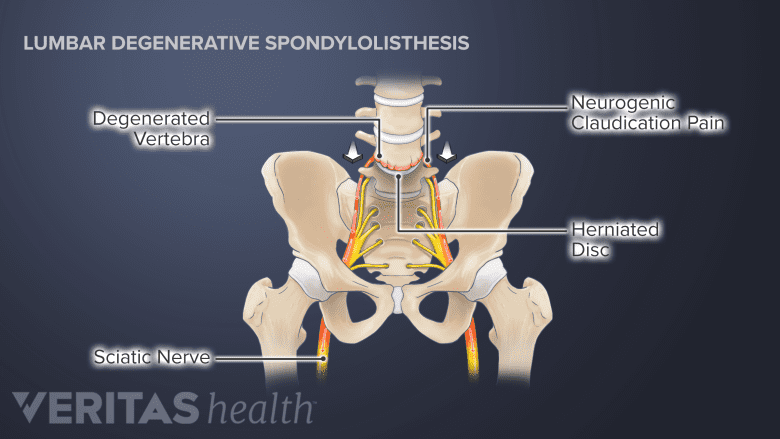
Degenerative spondylolisthesis is a common cause of neurogenic claudication.
This type of leg pain occurs due to narrowing of the spinal canal (spinal stenosis) causing compression of the spinal cord. This compression may occur due to bone spurs (abnormal bone growth), lumbar disc herniation, or spondylolisthesis (forward slippage of a vertebra).
The symptoms of neurogenic claudication typically occur in both legs and include9Munakomi S, Foris LA, Varacallo M. Spinal Stenosis And Neurogenic Claudication. [Updated 2019 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430872/:
- Pain and numbness while walking, standing, or performing upright exercises
- Weakness during leg movements
Neurogenic claudication pain typically increases while bending the spine backward and decreases while bending forward at the waist, sitting, or lying down.
A qualified medical professional can help diagnose the exact cause of nerve pain in the leg based on the type of presenting symptoms, medical history, and by performing certain clinical tests.
- 1 Alexander CE, Varacallo M. Lumbosacral Radiculopathy. [Updated 2019 Mar 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430837/
- 2 Wright R, Inbody SB. Radiculopathy and Degenerative Spine Disease. In: Neurology Secrets. Elsevier; 2010:121-130. doi:10.1016/b978-0-323-05712-7.00007-6
- 3 Harati Y, Kwan J, Smyth S. Peripheral Neuropathies and Motor Neuron Diseases. In: Neurology Secrets. Elsevier; 2010:97-120. doi:10.1016/b978-0-323-05712-7.00006-4
- 4 Callaghan BC, Price RS, Feldman EL. Distal Symmetric Polyneuropathy: A Review. JAMA. 2015;314(20):2172–2181. doi:10.1001/jama.2015.13611
- 5 Ng PS, Dyck PJ, Laughlin RS, Thapa P, Pinto MV, Dyck PJB. Lumbosacral radiculoplexus neuropathy. Neurology. February 2019:10.1212/WNL.0000000000007020. doi:10.1212/wnl.0000000000007020
- 6 Poage C, Roth C, Scott B. Peroneal Nerve Palsy. Journal of the American Academy of Orthopaedic Surgeons. 2016;24(1):1-10. doi:10.5435/jaaos-d-14-00420
- 7 Cheatham SW, Kolber MJ, Salamh PA. Meralgia paresthetica: a review of the literature. Int J Sports Phys Ther. 2013;8(6):883-93.
- 8 Kiel J, Kaiser K. Tarsal Tunnel Syndrome. [Updated 2019 Feb 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK513273/
- 9 Munakomi S, Foris LA, Varacallo M. Spinal Stenosis And Neurogenic Claudication. [Updated 2019 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430872/

