The underlying causes for most occurrences of back pain are non-emergent, but the intense pain and related symptoms often elevate anxiety and prompt a visit to the emergency room (ER). While back pain is typically treated in a primary care setting or by a musculoskeletal specialist, physicians are often cautious and look for warning signs of neurologically impairing or life-threatening causes. These causes are rare, but if present, they are considered a medical emergency and warrant immediate treatment to preserve back and/or leg function.
Back pain is considered the most common musculoskeletal cause for emergency room visits and typically involves individuals aged 18 to 65 years.1Corwell BN. The emergency department evaluation, management, and treatment of back pain. Emergency Medicine Clinics of North America. 2010;28(4):811-839. doi: 10.1016/j.emc.2010.06.001,2Pakpoor J, Raad M, Harris A, et al. Use of imaging during emergency department visits for low back pain. American Journal of Roentgenology. 2020;214(2):395-399. doi: 10.2214/AJR.19.21674
This article provides a comprehensive guide to when back pain may indicate a medical emergency and the associated red-flag symptoms to watch out for.
In This Article:
- When Back Pain May Be a Medical Emergency
- Back Pain Red-Flags for Emergency Room vs. Physician Consults
When an Emergency Room Visit Is Warranted for Back Pain
When dealing with severe back pain, making a judgment call about whether to seek help in a doctor’s office or visit the ER may be difficult.
The following list describes the symptoms and signs related to conditions that may have resulted in spinal cord, cauda equina, or internal organ damage, which are typically considered as a medical emergency.
Abdominal aortic aneurysm
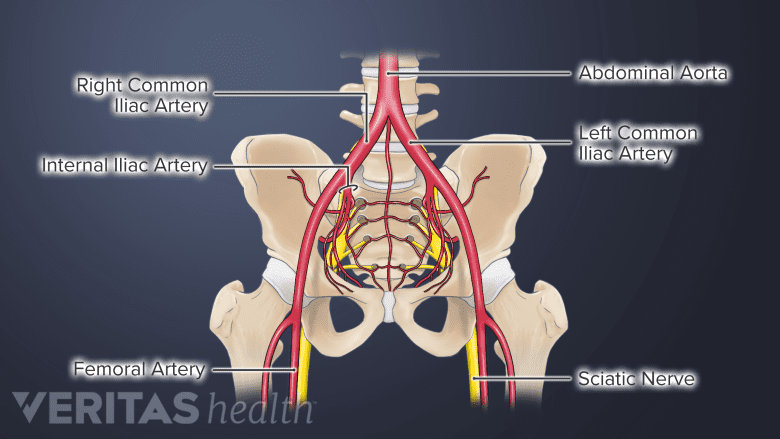
Rupture of the abdominal aorta is a serious medical condition.
Lower back pain that radiates to the front abdomen may occur together in a rare, serious medical condition called abdominal aortic aneurysm. Classic symptoms include:
- A continuous, stabbing pain of severe intensity felt deep in the abdomen between the sternum in the center of the chest and the belly button.
- Lower back pain, which may also spread to the groin, pelvis, and/or legs.
- A pulsating mass in the abdomen, which may be felt through the skin and is sensitive to touch.
- Sudden and rapid heartbeat, shallow breathing, clammy skin and cold sweats, general weakness, confusion, anxiety, and/or loss of consciousness, indicating shock.
Abdominal aneurysms are more prevalent among men aged 65 to 75 years who smoke cigarettes.3Fact Sheet: Abdominal Aortic Aneurysm. Center for Disease Control and Prevention Website. Updated Sept 08, 2020. Accessed January 15, 2021.
See Abdominal Aortic Aneurysm Causes
Cauda equina syndrome
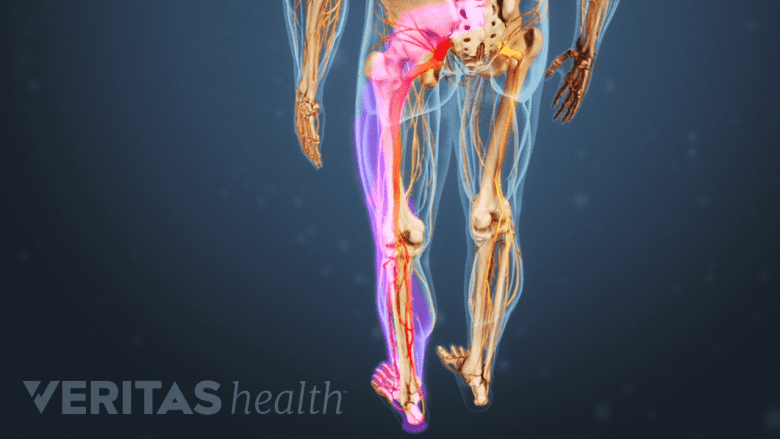
Damage to the cauda equina nerves can cause cauda equina syndrome, a condition that results in severe impairments in the lower back and leg(s). The hallmark symptoms of this condition include:
- Difficulty or inability to control bowel movements with sensory loss and decreased sphincter tone in the anal region4Kim K-H, Kim DH. Diagnosis and Treatment of Spinal Pain. In: Minimally Invasive Percutaneous Spinal Techniques. Elsevier; 2010:1-28.,5Fairbank J, Mallen C. Cauda equina syndrome: implications for primary care. Br J Gen Pract. 2014;64(619):67–68. doi:10.3399/bjgp14X676988
- Difficulty in passing urine, a reduced urinary sensation, a loss of desire to pass urine, and/or a poor stream4Kim K-H, Kim DH. Diagnosis and Treatment of Spinal Pain. In: Minimally Invasive Percutaneous Spinal Techniques. Elsevier; 2010:1-28.,5Fairbank J, Mallen C. Cauda equina syndrome: implications for primary care. Br J Gen Pract. 2014;64(619):67–68. doi:10.3399/bjgp14X676988
- Numbness in the groin, buttocks, genitals, and/or inner thighs (saddle numbness)3Fact Sheet: Abdominal Aortic Aneurysm. Center for Disease Control and Prevention Website. Updated Sept 08, 2020. Accessed January 15, 2021.
- Sexual dysfunction5Fairbank J, Mallen C. Cauda equina syndrome: implications for primary care. Br J Gen Pract. 2014;64(619):67–68. doi:10.3399/bjgp14X676988,6Verdugo RJ, Campero M, Castillo JL, Cea G. Pain and Temperature. In: Textbook of Clinical Neurology. Elsevier; 2007:363-381. doi:10.1016/b978-141603618-0.10020-7
Cauda equina syndrome may occur as a result of acute trauma or develop without an inciting event, due to the progression of an underlying condition. These conditions may include a lumbar herniated disc, lumbar spinal stenosis, or spinal tumor that affects the cauda equina nerves.
Read more about Causes of Cauda Equina Syndrome
Spinal tumor

Spinal tumors may cause neurologic complications.
Benign or metastatic spine tumors may cause back pain as the first symptom. Over time, they are typically accompanied by other distinguishing symptoms, such as:
- Unrelenting pain despite rest and medication
- Fever and chills
- Night pain
- Night sweats
- Progressive or sudden motor weakness in the leg(s)
- Unexplained weight loss
Tumors can originate in the spine or spread to the spine from other parts of the body, in which case they are more likely to lodge in the vertebrae because of the spine’s extensive network of blood vessels. The back and leg symptoms are typically dictated by the location of the tumor in the spine.
See Could My Back Pain Be Spine Cancer?
Spinal infection
Spinal infection may cause sciatica-like symptoms.
Harmful microorganisms can travel to the spine from other parts of the body where infection exists. The resulting spinal infection, called vertebral osteomyelitis, can result in back pain. The symptoms of a spinal infection are variable and depend on the age of the patient, the severity of the infection, and the location in the spine. In addition to back pain, spinal infection symptoms may include some combination of the following:
- Fever with chills
- Pain that is worse at night
- Swelling and possible warmth and redness around the infection site
- Unexplained weight loss
A spinal infection may move into the spinal canal and cause an epidural abscess, which can place pressure on the neural elements, such as the spinal cord, cauda equina, and/or spinal nerve roots. Depending on the level of infection and/or the degree of severity, sciatica-like symptoms, such as numbness, weakness, or paralysis, may occur in the areas of the body below the affected site.
Acute trauma

Back trauma may result in foot weakness, numbness, and functional loss.
Back pain that occurs immediately after acute trauma to the upper or lower back prompts urgent evaluation. Examples of acute trauma include sudden injuries from events like a slip, fall, playing active sports, or motor vehicle accident.
Moderate to severe back pain may develop as the only symptom or may occur in tandem with neurological symptoms, such as:
- Leg pain and numbness
- Inability to lift the foot (foot drop)
- Complete loss of sensation in one or both legs indicating paralysis
Injuries from acute trauma to the back can result in a spinal fracture or severe spondylolisthesis, which can compress or injure the spinal cord and/or cauda equina at the level involved. If an underlying bone-weakening condition, such as osteoporosis, exists, even mild trauma may cause compression fractures in the spine.
Who May Be Prone to Back Pain from Medical Emergencies

Individuals below 18 years and over 50 years of age are typically at a higher likelihood of serious back conditions.
While a serious medical condition can affect anyone, some individuals are more prone to these problems due to their underlying health conditions, physical characteristics, and lifestyle habits.
This list outlines the groups of people most prone to back pain from medical emergencies:
- The young and the elderly. The age of the individual is an important initial consideration when diagnosing back pain. Those less than 18 years or more than 50 years of age are typically at a higher likelihood of serious conditions as the cause for the back pain and typically need immediate care when symptoms occur.
- Tumors and infection occur with higher frequency in both these age groups.1Corwell BN. The emergency department evaluation, management, and treatment of back pain. Emergency Medicine Clinics of North America. 2010;28(4):811-839. doi: 10.1016/j.emc.2010.06.001
- Younger individuals are at increased risk of spondylolysis and spondylolisthesis.1 If these conditions are severe, they can affect the neural elements of the spine, causing pain and disability.
- Elderly individuals are more susceptible to abdominal aortic aneurysm.3Fact Sheet: Abdominal Aortic Aneurysm. Center for Disease Control and Prevention Website. Updated Sept 08, 2020. Accessed January 15, 2021.
- Older individuals may sustain fractures, including pathologic fractures, even with minor trauma.1Corwell BN. The emergency department evaluation, management, and treatment of back pain. Emergency Medicine Clinics of North America. 2010;28(4):811-839. doi: 10.1016/j.emc.2010.06.001
- The immunocompromised. Reduced immunity or a weakened immune system can make individuals susceptible to specific spinal conditions. Examples of the various causes of reduced immunity and the resultant back pain conditions that are likely to occur are outlined below1Corwell BN. The emergency department evaluation, management, and treatment of back pain. Emergency Medicine Clinics of North America. 2010;28(4):811-839. doi: 10.1016/j.emc.2010.06.001:
- A history of intravenous drug abuse, and/or recent bacterial infection, such as pneumonia or urinary tract infection, may pose an increased risk for spinal infection.
- Chronic steroid use and/or a history of cancer are linked to an increased risk for a spinal fracture, even from minor trauma.
- Cancer in another part of the body, especially in the breast, lung, or prostate, can metastasize in the spine, which is the third most common site for metastatic tumors.
As a general rule, any concerning symptom or sign needs to be evaluated by a medical professional. A trained medical professional can adequately evaluate the vital signs, prescribe the necessary diagnostic tests, identify potential neurologic defects, and uncover any red flags. Physicians can also provide timely treatment to prevent the progression of the condition, avoiding permanent damage to the tissues.
- 1 Corwell BN. The emergency department evaluation, management, and treatment of back pain. Emergency Medicine Clinics of North America. 2010;28(4):811-839. doi: 10.1016/j.emc.2010.06.001
- 2 Pakpoor J, Raad M, Harris A, et al. Use of imaging during emergency department visits for low back pain. American Journal of Roentgenology. 2020;214(2):395-399. doi: 10.2214/AJR.19.21674
- 3 Fact Sheet: Abdominal Aortic Aneurysm. Center for Disease Control and Prevention Website. Updated Sept 08, 2020. Accessed January 15, 2021.
- 4 Kim K-H, Kim DH. Diagnosis and Treatment of Spinal Pain. In: Minimally Invasive Percutaneous Spinal Techniques. Elsevier; 2010:1-28.
- 5 Fairbank J, Mallen C. Cauda equina syndrome: implications for primary care. Br J Gen Pract. 2014;64(619):67–68. doi:10.3399/bjgp14X676988
- 6 Verdugo RJ, Campero M, Castillo JL, Cea G. Pain and Temperature. In: Textbook of Clinical Neurology. Elsevier; 2007:363-381. doi:10.1016/b978-141603618-0.10020-7

