Your neck is a marvel of engineering – it supports your head while allowing it to move in all directions, houses sensitive nerves that connect to your arms and hands, while also providing protection for your spinal cord.
But your neck is also susceptible to and stiffness – ranging from a mild ache to severe, debilitating pain that radiates down your shoulder and arm.
Understanding neck pain and getting an accurate clinical diagnosis is key to effective treatment.
The medical term for neck pain is cervicalgia. This term derives from Latin and Greek terms:
- Cervic, meaning neck
- Algia, meaning pain
Types of Neck Pain
There are four main types of neck pain is typically diagnosed as one or a combination of four types of pain:
1. Axial Neck Pain
This type of neck pain is by far the most common. It is also referred to in the medical profession as mechanical neck pain, or nonspecific neck pain, and is commonly caused by a strained muscle.
Description:
- The pain is localized to one area of the neck without spreading to other areas of your body
- Feels dull, achy, throbbing, or sharp
- Worsens with certain movements or poor posture
Common Causes:
- Neck muscle strains or ligament sprains
- Spinal disc degeneration
- Trauma (e.g., vertebral fracture)
- Degeneration of the facet joints in the back of the spine (cervical osteoarthritis)
- Stresses due to posture, such as looking down at a device for long periods – sometimes called tech-neck, or large breasts that cause one to hunch forward
Axial neck pain can occur anywhere along the cervical spine, and it can affect multiple motion segments at one time. It tends to occur in the lower two motion segments, C4-C5, C5-C6 and C6-C7, as these segments have a lot of motion.
In This Article:
2. Cervical Radicular Pain
Pain that radiates from the neck down into the arm and/or hand is called radicular pain.
This occurs when the spinal nerve root, called a radicular nerve, is pinched or inflamed due to a condition in the cervical spine.
A nerve root problem can also cause a radiculopathy, which is the term used to describe nerve symptoms such as weakness, numbness or tingling that radiates along the path of the nerve.
Watch Cervical Radiculopathy Video
Description:
- Caused by nerve root inflammation
- Radiates from the neck to the shoulder, arm, or hand
- Feels like electric shocks, burning, or searing pain
- Worsens with certain movements or postures
- Typically affects only one side of the body
Common Causes:
- A cervical herniated disc pinches or inflames the nerve root
- Bone spurs due to spinal stenosis or osteoarthritis cause nerve root irritation
- A degenerated disc compresses the nerve root or causes inflammation around it
Radicular pain is commonly diagnosed in the lower motion segments in the cervical spine, the C5-C6 segment and the C6-C7 segment, although it can originate in any level.1Samir Sharrak; Yasir Al Khalili. Cervical Disc Herniation https://www.ncbi.nlm.nih.gov/books/NBK546618/. Last uodate August 28, 2023.
3. Referred Pain
Pain that is referred to the shoulder or other area of the body and is not radicular pain is called referred pain.
The area of distribution is likely to be more diffuse, or spread out, than radicular pain, but these two types of pain can feel similar. Referred pain is typically felt on only one side of the body, but it can be on both.
Description:
- Pain felt in an area other than its source
- Diffuse, deep, cramping, or throbbing sensation
- Typically felt on one side but can affect both
- Common referred pain travels from the neck to the head, shoulder, and/or upper back
Common Causes:
- Trigger points (sensitive muscle areas)
- Heart conditions (e.g., heart attack)
- Temporomandibular joint (TMJ) disorders
- Neck pathology leading to headache, shoulder, or upper back pain
The area of referred pain can be correlated with the level of the cervical spine that is affected.
For example, pain that is referred to the shoulder or the scapula (the large triangle-shaped shoulder bone at each side of your upper back) is usually correlated with a problem in the C5-C6 or C6-C7 cervical spine.
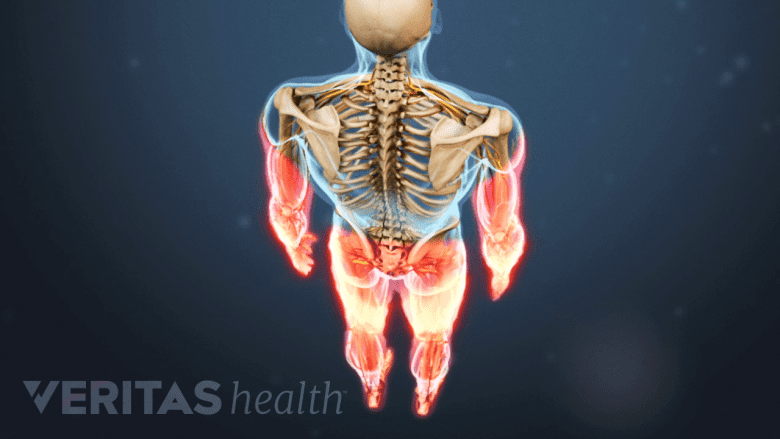
4. Myelopathic Pain
When the spinal cord in the neck becomes compressed, myelopathic pain may develop. This is commonly called cervical myelopathy.
While myelopathic pain may occur at the level of compression causing neck pain, symptoms are often located at a distance below the neck/compression site, such as in the legs and/or feet.
Description:
- Caused by spinal cord compression
- Symptoms tend to occur below the compression site (e.g., legs, feet)
- Symptoms depend on where and how the spinal cord is compressed
Symptoms:
- Myelopathy is commonly described as feeling like a deep ache, throbbing pain, and/or a cold or icy sensation
- May cause searing pain that feels like a shock running down the spine when the neck bends forward (Lhermitte’s sign)
- May mimic sciatica pain that radiates into the leg
Other terms used to describe myelopathy, such as tract pain and funicular pain, or cervical spondylotic myelopathy.
Any of these pain types can occur alone or in combination with one or more others. For example, it can be difficult to distinguish between radicular pain and referred pain, and some spinal pathologies can lead to both types of pain.
Acute vs. Chronic Neck Pain
Understanding how long pain lasts can help determine treatment:
| Pain Type | Duration | Common Causes |
|---|---|---|
| Acute | Less than 4 weeks | Injury (e.g., muscle strain, whiplash) |
| Subacute | > 4 weeks to 3 months | Lingering effects of injury |
| Chronic | 3+ months | Degenerative conditions or unknown causes |
Acute Neck Pain
Acute neck pain and stiffness tends to develop suddenly, and usually the trigger can be identified.
Common causes of acute neck pain:
- Poor sleeping posture and you wake up with a stiff neck
- Looking down at a mobile phone screen for long periods
- Carrying heavy bags on one shoulder
- Sudden trauma (e.g., whiplash or a sports injury)
Healing & Treatment:
- Usually resolves in days or weeks
- Treatments: ice/heat, massage, physical therapy, pain medication, anti-inflammatory medication (NSAIDs), rest, gentle stretching as tolerated
Chronic Neck Pain
Chronic neck pain may develop due to underlying conditions, such as disc degeneration, spinal stenosis or osteoarthritis. It may also start with an injury that doesn’t heal and leads to chronic pain.
Radiating neck pain with loss of balance and coordination warrants immediate medical attention.
When to Seek Prompt Medical Attention
Certain types of neck pain symptoms are caused by a serious underlying medical condition, such as a spinal cord compression, cancer, meningitis, or infections.
Neck pain requires immediate medical attention if it is accompanied by any of the following:
- Radiating pain into both arms or legs (myelopathic pain)
- Numbness, tingling, or weakness in arms or legs
- Problems with balance or coordination
- Loss of bowel or bladder control
- Unintended weight loss
- Fever or chills
- Severe headache with stiff neck
See When Is a Stiff Neck Serious?
When severe neck pain results from major trauma, such as a car accident or falling from a ladder, it must be treated as a medical emergency. To reduce the risk for paralysis, the patient should be immobilized by a medical professional and then transported to emergency care.
Final Thoughts
Neck pain is common among adults, but it can occur at any age. In the course of 3 months, about 15% of U.S. adults have neck pain that lasts at least one full day.
Knowing the type of neck pain you have helps guide effective and successful treatment.
- 1 Samir Sharrak; Yasir Al Khalili. Cervical Disc Herniation https://www.ncbi.nlm.nih.gov/books/NBK546618/. Last uodate August 28, 2023.

