Surgery for degenerative spondylolisthesis may be beneficial for select patients with lumbar radicular pain.
About 10% to 15% of individuals seeking treatment for degenerative spondylolisthesis eventually opt for surgical treatment. 1 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
In This Article:
- Degenerative Spondylolisthesis
- Degenerative Spondylolisthesis Symptoms
- Degenerative Spondylolisthesis Treatment
- Surgery for Degenerative Spondylolisthesis
- Degenerative Spondylolisthesis Video
Indications for Degenerative Spondylolisthesis Surgery
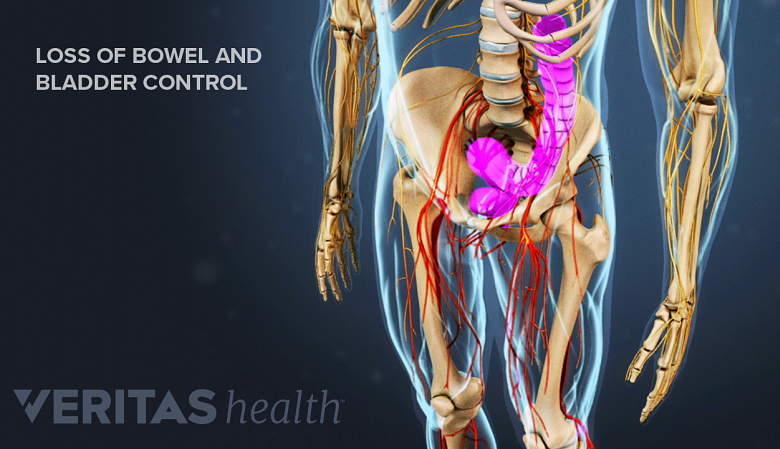
Loss of bowel and bladder control indicates a medical emergency.
Surgery for degenerative spondylolisthesis may be recommended when 2 Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008 Mar;17(3):327-335. doi: 10.1007/s00586-007-0543-3. Epub 2007 Nov 17. PMID: 18026865; PMCID: PMC2270383. :
- A series of nonsurgical treatments have been tried for a minimum of 3 to 6 months with no improvement in symptoms
- There is persistent or recurrent back and/or leg pain or neurogenic claudication
- The quality of life is significantly reduced
- There is progressive neurological deficit (more indicative of a surgical emergency)
- Bladder or bowel symptoms are present (more indicative of a surgical emergency)
See When Back Pain May Be a Medical Emergency
The goals of surgery are to stop progression of neurological deficits by alleviating pressure on nerve roots and the spinal nerves and provide stability to the area.
Success Rates of Surgical Treatment
Research shows that in appropriately selected patients, 66% to 96% of individuals may have successful outcomes, such as decreased pain and increased function, after surgery with a low rate of complications. 3 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed.; 2016. , 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
Some studies also suggest that long-term improvement in pain and function from surgical treatment is better than nonsurgical treatment, especially in patients with leg pain. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
Types of Surgeries for Degenerative Spondylolisthesis
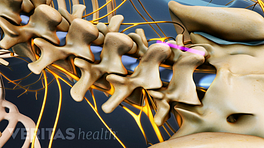
Lumbar laminectomy relieves neural compression by removing the bone compressing the nerve tissue.
Surgery for degenerative spondylolisthesis usually includes two parts, typically done together in one operation 5 Samuel AM, Moore HG, Cunningham ME. Treatment for Degenerative Lumbar Spondylolisthesis: Current Concepts and New Evidence. Curr Rev Musculoskelet Med. 2017 Dec;10(4):521-529. doi: 10.1007/s12178-017-9442-3. PMID: 28994028; PMCID: PMC5685964. , 6 Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/ :
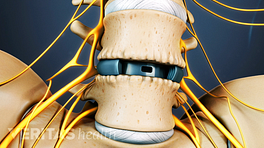
- Spinal decompression (also called a laminectomy), which helps relieve nerve root compression
- Spinal fusion with pedicle screw instrumentation and spinal interbody fusion, which helps improve the stability of the degenerated spinal segment
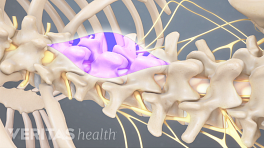
For single-level, low-grade degenerative spondylolisthesis with only central stenosis (narrowing of the spinal canal) and no foraminal stenosis (narrowing of the intervertebral foramen), decompression alone may provide equivalent outcomes compared to decompression with fusion.5
The additional step of spinal fusion with instrumentation is recommended to correct the deformity and prevent further progression of the condition. 7 Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(4):36917. doi: 10.52965/001c.36917. PMID: 35910544; PMCID: PMC9329062.
Interbody fusion may be used when the degree of slippage is higher and greater stability is needed. 7 Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(4):36917. doi: 10.52965/001c.36917. PMID: 35910544; PMCID: PMC9329062.
Considerations for Specific Interbody Fusion Approaches
The type of fusion depends on the underlying condition, skill, and experience of the surgeon, and the patient’s overall health.
- ALIF and XLIF are typically recommended for the restoration of the disc and foraminal height. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
- TLIF is typically recommended for increasing spinal canal cross-sectional area and relieving nerve compression. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
- XLIF may cause lesser intraoperative blood and muscle damage when compared with TLIF or PLIF. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009 However, the XLIF procedure may be associated with a risk of transient neurologic deficits. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
- TLIF and PLIF when performed as an open procedure may be associated with a higher risk of adjacent segment disease and subsidence. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
If the patient has undergone previous abdominal surgery, ALIF is usually not recommended. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
Open vs Minimally Invasive Surgery for Spondylolisthesis
Multiple studies have demonstrated that minimally invasive spine surgery yields similar clinical results to traditional open fusion while offering several notable benefits. These benefits include reduced costs, shorter operating times, decreased blood loss, and a shorter hospital stay. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
Due to these benefits, minimally invasive spine surgery may be more helpful for patients requiring a two-level fusion procedure. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
Potential Risks and Complications of Surgery
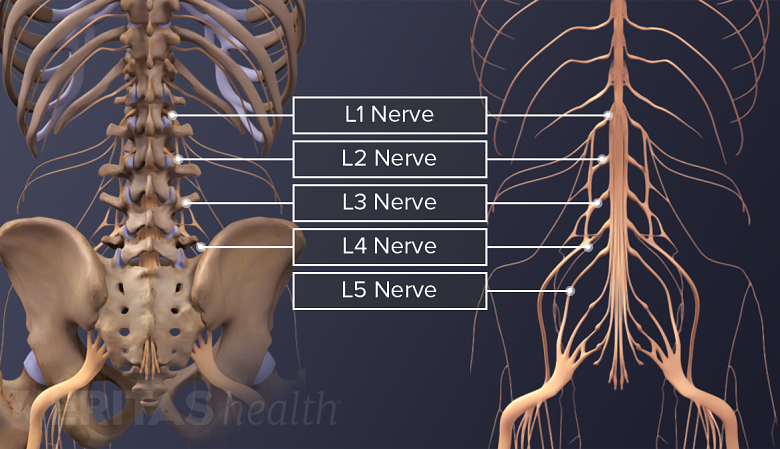
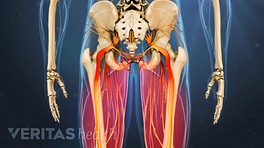
Damage to the lumbar spinal nerves is a potential risk of spinal surgery.
There are several potential risks and complications associated with degenerative spondylolisthesis surgery, which are typically the same for any fusion or decompression surgery.
Since degenerative spondylolisthesis is a condition that disproportionately affects older individuals, surgery may present some additional risk in this age group. Surgical risk is more directly related to the overall health of a patient and not his or her absolute age.
Potential risks and complications include:
- Fusion failure (arthrodesis)
- Hardware failure
- Continued pain
- Adjacent segment disease
- Infection
- Bleeding
- Dural leak
- Nerve root damage
These complications are usually rare, but increased risks can be seen in certain situations. Conditions that increase the risk of surgery include smoking (or any type of nicotine intake), obesity, multilevel fusions, osteoporosis (thinning of the bones), diabetes, rheumatoid arthritis, or prior failed back surgery.
See Failed Back Surgery Syndrome (FBSS): What It Is and How to Avoid Pain after Surgery
The surgeon must discuss the potential risks, benefits, and alternatives to surgery with the patient before surgical treatment is chosen.
- 1 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
- 2 Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008 Mar;17(3):327-335. doi: 10.1007/s00586-007-0543-3. Epub 2007 Nov 17. PMID: 18026865; PMCID: PMC2270383.
- 3 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed.; 2016.
- 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
- 5 Samuel AM, Moore HG, Cunningham ME. Treatment for Degenerative Lumbar Spondylolisthesis: Current Concepts and New Evidence. Curr Rev Musculoskelet Med. 2017 Dec;10(4):521-529. doi: 10.1007/s12178-017-9442-3. PMID: 28994028; PMCID: PMC5685964.
- 6 Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/
- 7 Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(4):36917. doi: 10.52965/001c.36917. PMID: 35910544; PMCID: PMC9329062.