Lumbar spinal fusion is a major surgery designed to stop the motion at a painful vertebral segment in the low back.
The objectives of spinal fusion are to1Formica M, Vallerga D, Zanirato A, Cavagnaro L, Basso M, Divano S, Mosconi L, Quarto E, Siri G, Felli L. Fusion rate and influence of surgery-related factors in lumbar interbody arthrodesis for degenerative spine diseases: a meta-analysis and systematic review. Musculoskelet Surg. 2020 Apr;104(1):1-15. doi: 10.1007/s12306-019-00634-x. Epub 2020 Jan 1. PMID: 31894472.:
- Attain a solid bony fusion that immobilizes the segment
- Improve spinal stability
- Correct anatomical deformities
- Relieve nerve compression
Spinal fusion is the preferred surgical approach for treating degenerative spine disorders2Reid PC, Morr S, Kaiser MG. State of the union: a review of lumbar fusion indications and techniques for degenerative spine disease. J Neurosurg Spine. 2019 Jul 1;31(1):1-14. doi: 10.3171/2019.4.SPINE18915 and may be performed via the traditional open surgical method or minimally invasive techniques.
In This Article:
- Lumbar Spinal Fusion Surgery
- Spine Fusion Risks and Complications
- Lumbar Spinal Fusion Surgery Animation
How Spinal Fusion Works in the Lower Back
The lumbar spine (low back) has 5 mobile spinal levels from L1 to S1, also known as motion segments. At each spinal level, motion is controlled by a disc and a pair of facet joints. The disc and motion segment are named by the vertebral body above and below; for example, the disc and motion segment related to the L4 and L5 vertebrae are called the L4-L5 disc and the L4-L5 motion segment.
Watch Understanding L5-S1 Spinal Fusion Animation
How spinal fusion sets up
A lumbar fusion surgery stops the motion at a painful motion segment. The fusion is not actually done at the time of the surgery; rather, the surgery sets up the conditions for the bone to heal across the spinal segment to form a bone to replace the joint. The bone healing process takes several months to over a year to fully set up.
After a spinal fusion surgery is performed, the following processes occur:
- A living bone bridge is formed between the two surrounding vertebrae.
- Depending on the surgical approach, this bridge develops either behind the disc between the posterior bony elements, through the disc space, or both.
- The bridge stiffens that segment in the spine and stops any motion at the fused motion segment.
- Spinal instrumentation (typically screw and rod fixation) is commonly used to secure the segments while the bony fusion forms.
Spinal fusion surgery may also include fusing the spinal facet joints for added stability.
Using a Bone Graft in Spinal Fusion
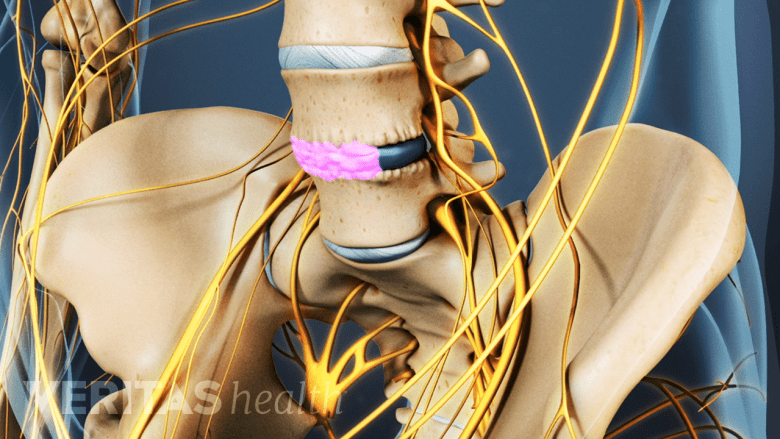
Bone graft aids in the growth of new bone and helps fuse the spinal motion segment.
It is common to use a bone graft to bridge the vertebral bones. The bone graft facilitates bone growth through and around the disc, fusing the spinal bones (vertebrae), and aiding in immobilizing the motion segment.
Bone graft materials can be the patient’s own bone (autograft), donor bone from a bone bank (allograft), or synthetic materials commonly populated with a patient’s bone marrow.
Due to their efficacy and safety, autografts are considered the gold standard for spinal fusions.3Lombardo JA, Russell N, He J, Larson MJ, Walsh WR, Mundis GM Jr, Vizesi F. Autograft Cellular Contribution to Spinal Fusion and Effects of Intraoperative Storage Conditions. Spine (Phila Pa 1976). 2023 Aug 15;48(16):1181-1189. doi: 10.1097/BRS.0000000000004688. Epub 2023 Apr 20. PMID: 37078877; PMCID: PMC10368216. However, there is some morbidity associated with bone graft harvest, and there is a limited supply of graft bone from the patient.
The Use of Cage Implants in Spinal Fusion
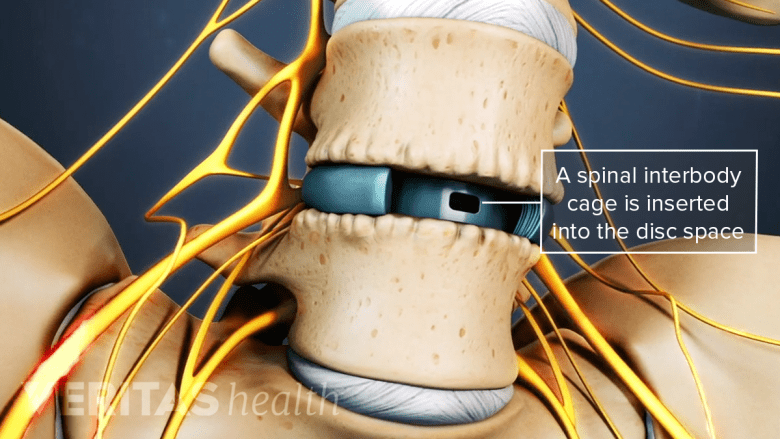
The spinal implants stabilize the spine, promote bone healing, and decompress nerves.
Interbody cage implants are designed to stop motion at the fusion segment to promote bone healing for fusion. They help support the front (anterior) part of the spinal segment, which bears 80% of the spinal loads, and dissipate forces placed on the rods and screws at the back.4Souslian FG, Patel PD. Review and analysis of modern lumbar spinal fusion techniques. Br J Neurosurg. 2021 Jul 15:1-7. doi: 10.1080/02688697.2021.1881041. Epub ahead of print. PMID: 34263676.
Spinal cages come in different shapes and sizes depending on the surgical approach and indication for spine fusion.
- Anterior spinal cages are used in anterior spinal approaches. They are available as a single piece and cover the entire disc space. They come in different sizes and wedge shapes to precisely fit into the disc space and reconstruct the normal spine shape. Some cages are designed to be implanted in a compressed state and expand once inside the disc space.
- Anterior cages can be implanted from the side of the spine (lateral approach) and from a modified anterior approach (anterior to the psoas muscle). The shapes of these cages are modified because of anatomic constraints but perform similarly to pure anterior cages.
- Posterior interbody cages are designed for the posterior (back) approach. They can be straight or crescent-shaped and expandable or fixed.
The goals of these implants are to stabilize the spine in an anatomic alignment, promote bone healing for fusion, indirectly decompress the nerves, and prevent injury to the normal tissues. Spinal cages can be placed by open or minimally invasive techniques.
Read more about Interbody Cages for Spine Fusion
The surgical decisions regarding approach and implants comprise several considerations. These include the reason for surgery (indication), the patient’s anatomy, prior surgery or medical intervention (eg, radiation therapy), the surgeon’s skill, and hospital/surgical center capabilities.
Spinal fusion surgery may be considered when abnormal and excessive motion at a vertebral segment results in severe pain and inability to function. The surgery aims to stabilize the spine in a position that is close to normal, thereby preventing any abnormal rotation, nerve compression, and pain.4Souslian FG, Patel PD. Review and analysis of modern lumbar spinal fusion techniques. Br J Neurosurg. 2021 Jul 15:1-7. doi: 10.1080/02688697.2021.1881041. Epub ahead of print. PMID: 34263676.
Indications for spinal fusion include5Benzon HT, Raja S, Liu SS, Fishman S, Cohen SP, eds. Essentials of Pain Medicine. Fourth edition. Elseiver; 2018.:
- Spondylolisthesis
- Spondylolysis
- Spinal stenosis
- Degenerative disc disease
- Discogenic pain or pain originating from a spinal disc
- Spinal instability during surgery or from a past decompressive surgery, such as lumbar laminectomy
- Medical emergencies, such as a tumor and certain types of traumas
Spine fusion is also indicated to treat spinal deformities, such as scoliosis. Unless a medical emergency, a series of nonsurgical treatments are usually tried before spinal fusion surgery is considered.
Interbody Fusions of the Lumbar Spine
An interbody spinal fusion involves removing the intervertebral disc and inserting an implant or bone graft in the disc space. This implant or bone graft helps restore disc height, relieve nerve compression, and facilitate bone growth for fusion.6Verma R, Virk S, Qureshi S. Interbody Fusions in the Lumbar Spine: A Review. HSS J. 2020 Jul;16(2):162-167. doi: 10.1007/s11420-019-09737-4. Epub 2020 Jan 13. PMID: 32523484; PMCID: PMC7253570.
Lumbar interbody fusion can be performed through various approaches:
- Posterior lumbar interbody fusion (PLIF): the spine is approached through the back
- Anterior lumbar interbody fusion (ALIF): the spine is approached through the abdomen
- Transforaminal lumbar interbody fusion (TLIF): the spine is approached from the back through the hollow bony openings (foramina) between adjacent spinal segments
- Extreme lateral interbody fusion (XLIF): the spine is approached from the side
Interbody fusion surgeries are among the most common types of spinal fusion surgery.6Verma R, Virk S, Qureshi S. Interbody Fusions in the Lumbar Spine: A Review. HSS J. 2020 Jul;16(2):162-167. doi: 10.1007/s11420-019-09737-4. Epub 2020 Jan 13. PMID: 32523484; PMCID: PMC7253570.
Posterolateral Gutter Fusion
A posterolateral gutter fusion is performed via a posterior (back) approach. In this method, the bone graft is placed in a region outside the spine, near the paired facet joints and the intertransverse gutter. This approach allows clear surgical access over multiple spinal levels.7Cruz A, Ropper AE, Xu DS, Bohl M, Reece EM, Winocour SJ, Buchanan E, Kaung G. Failure in Lumbar Spinal Fusion and Current Management Modalities. Semin Plast Surg. 2021 Feb;35(1):54-62. doi: 10.1055/s-0041-1726102. Epub 2021 May 10. PMID: 33994880; PMCID: PMC8110346.
Due to its position, the bone graft in a posterolateral approach is not load-bearing but rather placed under tension.7Cruz A, Ropper AE, Xu DS, Bohl M, Reece EM, Winocour SJ, Buchanan E, Kaung G. Failure in Lumbar Spinal Fusion and Current Management Modalities. Semin Plast Surg. 2021 Feb;35(1):54-62. doi: 10.1055/s-0041-1726102. Epub 2021 May 10. PMID: 33994880; PMCID: PMC8110346.
An interbody fusion may be performed along with the posterolateral gutter surgery if restoration of disc height is needed.7Cruz A, Ropper AE, Xu DS, Bohl M, Reece EM, Winocour SJ, Buchanan E, Kaung G. Failure in Lumbar Spinal Fusion and Current Management Modalities. Semin Plast Surg. 2021 Feb;35(1):54-62. doi: 10.1055/s-0041-1726102. Epub 2021 May 10. PMID: 33994880; PMCID: PMC8110346.
Anterior and Posterior Spinal Fusion
The anterior and posterior fusion procedure, also called a 360° or circumferential fusion, involves fusing both the front and back of the spine to provide a high degree of stability and a large surface area for the bone fusion to occur.
Multilevel Spinal Fusion

Multilevel spinal fusions are more common in the lower lumbar segments.
A multilevel spinal fusion involves fusing two or more levels of the spine, such as the L4-L5 and L5-S1 spinal segments. Multilevel fusions considerably limit the normal motion in the lower back and place more stress across the remaining mobile joints.
Watch Stages of Bone Healing in Lumbar Spine Fusion Surgery Video
Fusing 3 or more levels of the spine is rare and usually reserved for the treatment of scoliosis or lumbar deformity.
Spinal Instrumentation to Secure the Fused Vertebrae
Spinal fusion typically involves the use of some form of spinal instrumentation, which helps provide additional spinal stability, acting as an internal brace while the bony fusion heals.
Common surgical implants used in spine fusion include spinal interbody cages, anterior plates, pedicle screws and rods, hooks, and wires.
Success Rates of Lumbar Spinal Fusion Surgery
Research indicates that 65% to 95% of lumbar spinal fusions are successful.1Formica M, Vallerga D, Zanirato A, Cavagnaro L, Basso M, Divano S, Mosconi L, Quarto E, Siri G, Felli L. Fusion rate and influence of surgery-related factors in lumbar interbody arthrodesis for degenerative spine diseases: a meta-analysis and systematic review. Musculoskelet Surg. 2020 Apr;104(1):1-15. doi: 10.1007/s12306-019-00634-x. Epub 2020 Jan 1. PMID: 31894472.
The posterior lumbar interbody fusion (PLIF) approach typically has the highest rate of successful fusion and the lowest rate of complications compared to the other approaches.4Souslian FG, Patel PD. Review and analysis of modern lumbar spinal fusion techniques. Br J Neurosurg. 2021 Jul 15:1-7. doi: 10.1080/02688697.2021.1881041. Epub ahead of print. PMID: 34263676.
See PLIF Potential Advantages and Disadvantages
However, recent lumbar fusion studies demonstrate the superiority of ALIF, XLIF, and minimally invasive TLIF surgeries in regard to surgical outcomes, including pain relief, function, patient satisfaction, and recovery.8Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015 Dec;1(1):2-18. doi: 10.3978/j.issn.2414-469X.2015.10.05. PMID: 27683674; PMCID: PMC5039869.
Success rates based on specific conditions
The effectiveness of spinal fusion surgery varies depending on the underlying condition.5Benzon HT, Raja S, Liu SS, Fishman S, Cohen SP, eds. Essentials of Pain Medicine. Fourth edition. Elseiver; 2018.
- Favorable outcomes are generally reported when spinal fusion is used to treat spinal deformities and spondylolisthesis.5Benzon HT, Raja S, Liu SS, Fishman S, Cohen SP, eds. Essentials of Pain Medicine. Fourth edition. Elseiver; 2018.
- Modest outcomes have been reported when spinal fusion is used to treat degenerative disc disease and disc-related pain.5Benzon HT, Raja S, Liu SS, Fishman S, Cohen SP, eds. Essentials of Pain Medicine. Fourth edition. Elseiver; 2018.
The vast majority of fusion surgeries are typically considered for the treatment of degenerative spondylolisthesis, a condition where a vertebra slips over the vertebra below it due to age-related changes in the spine.9Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in Lumbar Fusion Procedure Rates and Associated Hospital Costs for Degenerative Spinal Diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976). 2019 Mar 1;44(5):369-376. doi: 10.1097/BRS.0000000000002822. PMID: 30074971.
Factors That Influence a Successful Fusion
Obtaining a successful result from a spine fusion requires several factors, including:
- Presurgical factors:
- An accurate diagnosis of the underlying condition
- A technologically adept, skilled surgeon
- Appropriate patient selection, taking into consideration the patient’s age, concomitant medical conditions, and lifestyle (healthy weight, does not smoke or use nicotine products)
- History of previous surgeries
- Surgical factors:
- Extent and type of surgery
- The use of hardware and instrumentation
- Number of levels fused
- Postsurgical factors:
- Compliance with postsurgical protocols
- How closely the care instructions are followed
Additionally, patients with malnutrition, depression, long-standing use of opioids before surgery, and use of chronic steroid medications, including prednisone, may be at risk of slower recovery after fusion surgery.
Patients and caregivers are advised to discuss the surgical procedure and recovery process in detail with the surgeon to get a thorough understanding of what to expect before and after surgery.
- 1 Formica M, Vallerga D, Zanirato A, Cavagnaro L, Basso M, Divano S, Mosconi L, Quarto E, Siri G, Felli L. Fusion rate and influence of surgery-related factors in lumbar interbody arthrodesis for degenerative spine diseases: a meta-analysis and systematic review. Musculoskelet Surg. 2020 Apr;104(1):1-15. doi: 10.1007/s12306-019-00634-x. Epub 2020 Jan 1. PMID: 31894472.
- 2 Reid PC, Morr S, Kaiser MG. State of the union: a review of lumbar fusion indications and techniques for degenerative spine disease. J Neurosurg Spine. 2019 Jul 1;31(1):1-14. doi: 10.3171/2019.4.SPINE18915
- 3 Lombardo JA, Russell N, He J, Larson MJ, Walsh WR, Mundis GM Jr, Vizesi F. Autograft Cellular Contribution to Spinal Fusion and Effects of Intraoperative Storage Conditions. Spine (Phila Pa 1976). 2023 Aug 15;48(16):1181-1189. doi: 10.1097/BRS.0000000000004688. Epub 2023 Apr 20. PMID: 37078877; PMCID: PMC10368216.
- 4 Souslian FG, Patel PD. Review and analysis of modern lumbar spinal fusion techniques. Br J Neurosurg. 2021 Jul 15:1-7. doi: 10.1080/02688697.2021.1881041. Epub ahead of print. PMID: 34263676.
- 5 Benzon HT, Raja S, Liu SS, Fishman S, Cohen SP, eds. Essentials of Pain Medicine. Fourth edition. Elseiver; 2018.
- 6 Verma R, Virk S, Qureshi S. Interbody Fusions in the Lumbar Spine: A Review. HSS J. 2020 Jul;16(2):162-167. doi: 10.1007/s11420-019-09737-4. Epub 2020 Jan 13. PMID: 32523484; PMCID: PMC7253570.
- 7 Cruz A, Ropper AE, Xu DS, Bohl M, Reece EM, Winocour SJ, Buchanan E, Kaung G. Failure in Lumbar Spinal Fusion and Current Management Modalities. Semin Plast Surg. 2021 Feb;35(1):54-62. doi: 10.1055/s-0041-1726102. Epub 2021 May 10. PMID: 33994880; PMCID: PMC8110346.
- 8 Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015 Dec;1(1):2-18. doi: 10.3978/j.issn.2414-469X.2015.10.05. PMID: 27683674; PMCID: PMC5039869.
- 9 Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in Lumbar Fusion Procedure Rates and Associated Hospital Costs for Degenerative Spinal Diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976). 2019 Mar 1;44(5):369-376. doi: 10.1097/BRS.0000000000002822. PMID: 30074971.

