There are three steps involved in the diagnosis of a lumbar (lower back) herniated disc: a medical history, a physical exam, and – when appropriate – advanced diagnostic testing.
A set of simple physical assessments, such as the straight leg raise test, allows the physician to determine whether a herniated disc is likely the cause of pain and where it is located.
Magnetic resonance imaging (MRI) is the gold standard imaging test for diagnosing a herniated disc, and these scans are considered when a clinical examination fails to determine a clear diagnosis.1Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/ MRI can also help rule out non-spinal causes of pain. Other tests such as nerve function testing (nerve conduction studies and electromyography) are used to determine the severity of nerve damage and its progression.
In This Article:
What to Expect During a Doctor’s Visit for a Herniated Disc
The initial clinical evaluation is designed to assess the nature and location of pain and observe any changes in tendon reflexes, sensation, muscle strength, or the range of motion.1Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/,2Donnally III CJ, Butler AJ, Varacallo M. Lumbosacral Disc Injuries. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448072/,3Tamarkin RG, Isaacson AC. Electrodiagnostic Evaluation of Lumbosacral Radiculopathy. [Updated 2022 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563224/
1. Medical history review
During a doctor’s visit, specific questions are asked about the nature of the symptoms, which may include:
- The onset of pain and other symptoms, such as numbness or weakness
- Type, nature, and duration of pain, such as localized or radiating, sharp or dull, constant or intermittent
- Any history of trauma or injury to the back or hip area
- Activities that worsen the symptoms or make it better
- Any changes in bladder or bowel function
Clear communication about symptoms with as much detail as possible helps physicians make a more accurate diagnosis.
Any experience with depression or anxiety should also be part of the discussion, as this information is helpful in planning treatment.
2. Physical exam
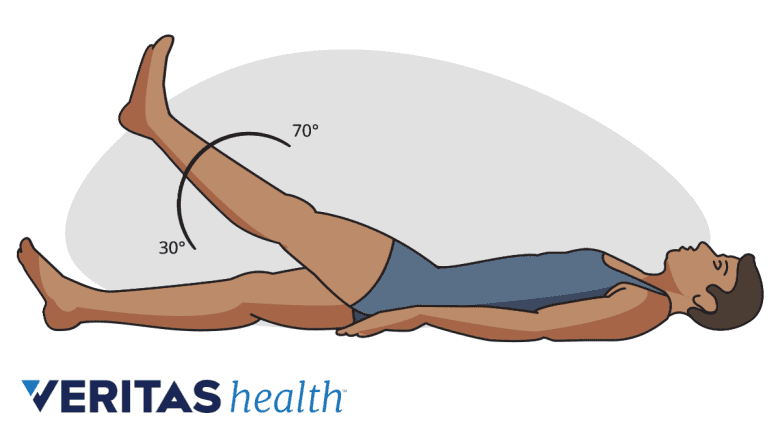
Flaring of low back pain during a straight leg raise test indicates a pinched lumbar nerve.
A physical exam involves the doctor checking the lower back and conducting clinical tests to evaluate the strength of the lower back and legs.
- Skin exam. The doctor checks the skin over the lower back for signs and symptoms of inflammation, abnormal texture or appearance, or an area that is tender or sensitive to touch.1Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/,2Donnally III CJ, Butler AJ, Varacallo M. Lumbosacral Disc Injuries. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448072/
- Lumbar spine exam. The patient’s standing and sitting postures are evaluated along with range of motion testing while bending backward, forward, and during spinal rotation.
Other surrounding joints, such as the hip joints and sacroiliac (SI) joints, are also evaluated. - Straight leg raise test. In this part of the exam, the patient lies down on his or her back and the doctor assists in raising the leg with painful symptoms without bending it. If this movement induces or worsens pain in the leg that is raised, it suggests irritation or compression of a sciatic nerve root. This test is particularly useful in diagnosing a lumbar disc herniation in either of the two lower levels of the lumbar spine, the L4-L5 spinal segment and the L5-S1 spinal segment.1Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/,2Donnally III CJ, Butler AJ, Varacallo M. Lumbosacral Disc Injuries. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448072/
The straight leg test is also referred to as the Laseque sign. - Crossed straight leg test. This test is a variation of the straight leg raise test and involves raising the leg that does not have painful symptoms. If raising this leg produces pain in the opposite (non-raised) leg, it suggests irritation or compression of a sciatic nerve root.1Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/,2Donnally III CJ, Butler AJ, Varacallo M. Lumbosacral Disc Injuries. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448072/
This test may also be referred to as the Fajersztajn sign or the “well-leg” raise test. - Reflex checks. Tendon reflexes on the affected leg are checked by tapping a tendon on the leg and/or foot with a reflex hammer. A lack of reflex response helps the doctor determine specific nerve root involvement and pinpoint the level of possible herniation.1Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/,2Donnally III CJ, Butler AJ, Varacallo M. Lumbosacral Disc Injuries. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448072/
These tests require a well-qualified spine specialist to interpret and make an accurate diagnosis.
3. Advanced diagnostic testing
For individuals who have a loss of deep tendon reflexes or significant numbness, advanced neurologic tests are usually performed.1Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/,3Tamarkin RG, Isaacson AC. Electrodiagnostic Evaluation of Lumbosacral Radiculopathy. [Updated 2022 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563224/
Sometimes, laboratory tests are used to measure levels of inflammatory and immune markers, including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), when there is concern that a chronic inflammatory condition or infection is the cause of pain.1Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/
When Imaging Tests Are Recommended
Diagnostic imaging may be recommended if there is no improvement in symptoms after 2 to 3 months of non-surgical treatments.1Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/ However, these tests may be recommended sooner if there are other concerns, such as symptoms that occur after an acute injury or trauma or if there are symptoms of cauda equina syndrome or other neurological concerns.
Imaging tests may be done sooner to rule out alternative causes of pain, such as fracture or infection. Imaging tests are routinely done prior to surgery for a herniated disc.1Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/
Magnetic resonance imaging (MRI)
MRI is the gold standard imaging test to confirm a herniated lumbar disc as it provides the most accurate assessment of the location of the herniation and affected neural tissue. MRI is also the preferred test for surgical planning.1Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/
X-ray
X-rays only show bones and don’t image soft tissues, such as discs. However, they may be needed to check for problems that involve the spinal bones, such as vertebral fractures or spondylolisthesis.
CT with myelogram
A computed tomography (CT) scan with myelogram is performed on patients who are unable to have an MRI. CT myelography is useful in evaluating soft tissues such as the discs, nerve roots, and the spinal cord or cauda equina.
- 1 Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/
- 2 Donnally III CJ, Butler AJ, Varacallo M. Lumbosacral Disc Injuries. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448072/
- 3 Tamarkin RG, Isaacson AC. Electrodiagnostic Evaluation of Lumbosacral Radiculopathy. [Updated 2022 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563224/

