The sacroiliac (SI) joints connect the sacrum at the base of the spine to the hip bone. They provide a great deal of strength to modulate powerful forces between the upper and lower body.1Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. doi:10.1111/j.1469-7580.2012.01564.x,2Wong M, Sinkler MA, Kiel J. Anatomy, Abdomen and Pelvis, Sacroiliac Joint. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507801/ These joints also protect the lowest motion segment of the spine, L5-S1, through their limited motion and the very strong ligaments that interconnect with the L5-S1 segment.
An extensive architecture of tough and resilient ligaments helps support the sacroiliac joints, permitting stable, yet flexible support to the upper body.
In This Article:
- Sacroiliac Joint Anatomy
- Sacroiliac Joint Ligaments and Muscles
- Sacroiliac (SI) Joint Anatomy Video
The Role of the Sacroiliac Joints: Stabilization, Shock Absorption, and Mobility

The SI joints are crucial for mobility, balance, and lower back function.
The sacroiliac joints provide a range of essential functions, which:
- Control and distribute the forces from the upper body into the legs.2Wong M, Sinkler MA, Kiel J. Anatomy, Abdomen and Pelvis, Sacroiliac Joint. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507801/
- Act as a shock absorber for the spine and control the transmission of forces from the lower body into the spine, such as gravitational forces and forces transmitted upward during standing or walking.2Wong M, Sinkler MA, Kiel J. Anatomy, Abdomen and Pelvis, Sacroiliac Joint. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507801/,4Cramer, Gregory D., and Chae-Song Ro. "The Sacrum, Sacroiliac Joint, and Coccyx." Clinical Anatomy of the Spine, Spinal Cord, and Ans, Elsevier, 2014, pp. 312–39. DOI.org (Crossref), doi:10.1016/B978-0-323-07954-9.00008-6
- Allow walking, spinal and thigh movements, and changes in posture or position, such as changing from lying to standing and standing to sitting.3Eshed, Iris, et al. "Peripartum Changes of the Sacroiliac Joints on MRI: Increasing Mechanical Load Correlating with Signs of Edema and Inflammation Kindling Spondyloarthropathy in the Genetically Prone." Clinical Rheumatology, vol. 34, no. 8, Aug. 2015, pp. 1419–26. DOI.org (Crossref), doi:10.1007/s10067-015-2976-0
- Support the weight of the upper body.3Eshed, Iris, et al. "Peripartum Changes of the Sacroiliac Joints on MRI: Increasing Mechanical Load Correlating with Signs of Edema and Inflammation Kindling Spondyloarthropathy in the Genetically Prone." Clinical Rheumatology, vol. 34, no. 8, Aug. 2015, pp. 1419–26. DOI.org (Crossref), doi:10.1007/s10067-015-2976-0
- Facilitate pregnancy and childbirth in women by widening and becoming more mobile.3Eshed, Iris, et al. "Peripartum Changes of the Sacroiliac Joints on MRI: Increasing Mechanical Load Correlating with Signs of Edema and Inflammation Kindling Spondyloarthropathy in the Genetically Prone." Clinical Rheumatology, vol. 34, no. 8, Aug. 2015, pp. 1419–26. DOI.org (Crossref), doi:10.1007/s10067-015-2976-0
The nervous system connections to this joint transmit pain signals arising from within the joint and its surrounding ligaments. The nerves also provide a sense of position and balance.4Cramer, Gregory D., and Chae-Song Ro. "The Sacrum, Sacroiliac Joint, and Coccyx." Clinical Anatomy of the Spine, Spinal Cord, and Ans, Elsevier, 2014, pp. 312–39. DOI.org (Crossref), doi:10.1016/B978-0-323-07954-9.00008-6
Sacroiliac Joint Articulation, Location, and Shape

The SI joints connect the spine to the pelvis and help transfer forces between the spine and legs.
The articulation between the outer side of the spine’s sacrum and the inner side of the butterfly-shaped hip bone (ilium) forms the sacroiliac joint.4Cramer, Gregory D., and Chae-Song Ro. "The Sacrum, Sacroiliac Joint, and Coccyx." Clinical Anatomy of the Spine, Spinal Cord, and Ans, Elsevier, 2014, pp. 312–39. DOI.org (Crossref), doi:10.1016/B978-0-323-07954-9.00008-6
- The SI joints are located on either side of the sacral spine and are situated deep in the pelvis.
- Each SI joint is secured and well protected by strong ligaments.
- The joint surface extends from the S1 spinal segment to the middle of the S3 spinal segment. This location may vary slightly, beginning above the S1 spinal segment (near L5-S1 or lumbosacral joint) and ending toward the top of the S3 spinal segment.4Cramer, Gregory D., and Chae-Song Ro. "The Sacrum, Sacroiliac Joint, and Coccyx." Clinical Anatomy of the Spine, Spinal Cord, and Ans, Elsevier, 2014, pp. 312–39. DOI.org (Crossref), doi:10.1016/B978-0-323-07954-9.00008-6
When viewed from the front, the joints are aligned in a parallel fashion on either side of the lower spine.
Directly pressing the skin over the sacroiliac joint in the rear pelvic area may elicit pain if the joint is inflamed (sacroiliitis) or not functioning as usual (sacroiliac joint dysfunction).
Articular Surface of the Sacroiliac Joint: Characteristics and Function

The SI joint is surrounded by a tough capsule that contains a lubricating fluid.
The unique sacroiliac articulation between the sacrum and the hip provides a transition between the spine and the pelvis.
While the SI joint has the features of a typical moveable joint, the movements within the joint are very limited.
The sacroiliac joint has a C-shaped contour
A fully developed adult sacroiliac joint is formed by two C-shaped (or inverted L-shaped) layers of bone with several irregular ridges and depressions.1Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. doi:10.1111/j.1469-7580.2012.01564.x
- The outer (convex) part of the C corresponds to the hip’s ilium bone. This surface is covered with thick hyaline cartilage.1Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. doi:10.1111/j.1469-7580.2012.01564.x
- The inner (concave) part of the C corresponds to the fused sacral bones S1-S3. This surface is lined with thin fibrocartilage.1Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. doi:10.1111/j.1469-7580.2012.01564.x
- In the sacroiliac joint, both types of cartilage have rough and coarse texture due to natural adaptation to stress.5Yoo WG. Effects of individual strengthening exercises for the stabilization muscles on the nutation torque of the sacroiliac joint in a sedentary worker with nonspecific sacroiliac joint pain. J Phys Ther Sci. 2015;27(1):313-314. doi:10.1589/jpts.27.313
- Both of these opposing joint surfaces articulate closely with each other.1Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. doi:10.1111/j.1469-7580.2012.01564.x
- The joint surface can be divided into 3 regions that correspond with the sacral vertebrae. The region near S1 is the largest and the joint surface near S3 is the smallest.1Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. doi:10.1111/j.1469-7580.2012.01564.x
The angle and texture of the connecting surfaces change mildly with age to overcome and resist forces and compression in this region.1Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. doi:10.1111/j.1469-7580.2012.01564.x The ridges and depressions along the joint’s surfaces develop and deepen with age.2Wong M, Sinkler MA, Kiel J. Anatomy, Abdomen and Pelvis, Sacroiliac Joint. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507801/
Joint Capsule and Synovial Fluid of the Sacroiliac Joint
The outer part of the SI joint is covered by a joint capsule made up of thick and tough membranous tissue. The inner portion of this capsule has a delicate lining membrane called the synovial membrane. This membrane secretes a fluid called the synovial fluid, which helps lubricate the joint.4Cramer, Gregory D., and Chae-Song Ro. "The Sacrum, Sacroiliac Joint, and Coccyx." Clinical Anatomy of the Spine, Spinal Cord, and Ans, Elsevier, 2014, pp. 312–39. DOI.org (Crossref), doi:10.1016/B978-0-323-07954-9.00008-6
The presence of this joint capsule and inner membrane classifies the SI joint into synovial and diarthrodial, which means moveable joint. The fibrous joint capsule is located along the front part of the sacroiliac joint and there is no capsule along the back of the joint. For this reason, some researchers classify the sacroiliac joint as an atypical synovial joint3Eshed, Iris, et al. "Peripartum Changes of the Sacroiliac Joints on MRI: Increasing Mechanical Load Correlating with Signs of Edema and Inflammation Kindling Spondyloarthropathy in the Genetically Prone." Clinical Rheumatology, vol. 34, no. 8, Aug. 2015, pp. 1419–26. DOI.org (Crossref), doi:10.1007/s10067-015-2976-0 or a modified synarthrodial joint.5Yoo WG. Effects of individual strengthening exercises for the stabilization muscles on the nutation torque of the sacroiliac joint in a sedentary worker with nonspecific sacroiliac joint pain. J Phys Ther Sci. 2015;27(1):313-314. doi:10.1589/jpts.27.313
The outer portion of this capsule is thick and tough.
Sacroiliac Joint Movement
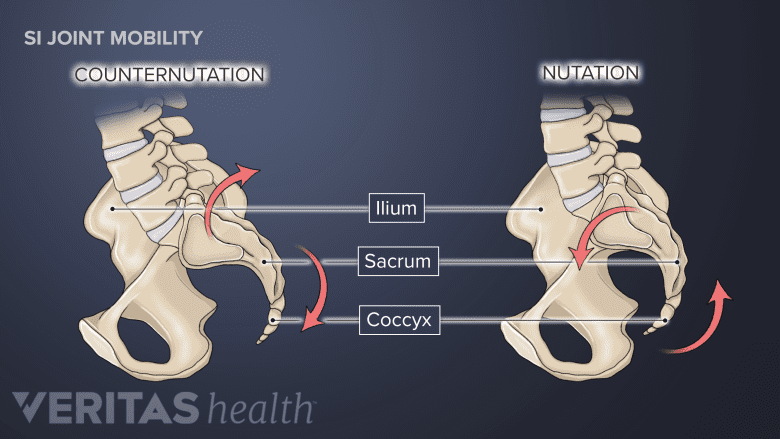
A normal SI joint can move forward and downward (nutation) and backward and upward (counternutation).
The primary movements within the sacroiliac joint are front-and-back (anterior-posterior). Movements also occur along different planes, such as upward and downward. Movements can be further grouped into:
- Nutation, which refers to the forward and downward (anterior-inferior) movement of the sacroiliac joint. The tailbone (coccyx) moves back in relation to the hip bone during this motion.2Wong M, Sinkler MA, Kiel J. Anatomy, Abdomen and Pelvis, Sacroiliac Joint. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507801/ The stability of the sacroiliac joint is increased by the nutation movement.5Yoo WG. Effects of individual strengthening exercises for the stabilization muscles on the nutation torque of the sacroiliac joint in a sedentary worker with nonspecific sacroiliac joint pain. J Phys Ther Sci. 2015;27(1):313-314. doi:10.1589/jpts.27.313
- Counternutation, which refers to the backward and upward (posterior-superior) movement of the joint. The tailbone moves forward in relation to the hip bone during this motion.2Wong M, Sinkler MA, Kiel J. Anatomy, Abdomen and Pelvis, Sacroiliac Joint. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507801/
These movements are typically limited to 2 mm to 4 mm and 2° to 5° due to the bony architecture and the surrounding ligaments of the joint.2Wong M, Sinkler MA, Kiel J. Anatomy, Abdomen and Pelvis, Sacroiliac Joint. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507801/,4Cramer, Gregory D., and Chae-Song Ro. "The Sacrum, Sacroiliac Joint, and Coccyx." Clinical Anatomy of the Spine, Spinal Cord, and Ans, Elsevier, 2014, pp. 312–39. DOI.org (Crossref), doi:10.1016/B978-0-323-07954-9.00008-6,6Ombregt, Ludwig. "Disorders of the Sacroiliac Joint." A System of Orthopaedic Medicine, Elsevier, 2013, pp. 603-610.e2. DOI.org (Crossref), doi:10.1016/B978-0-7020-3145-8.00043-0
A full range of motion of the sacroiliac joint is expressed when the extremes of hip motion are reached (such as while rotating the hip outward until the farthest point).4Cramer, Gregory D., and Chae-Song Ro. "The Sacrum, Sacroiliac Joint, and Coccyx." Clinical Anatomy of the Spine, Spinal Cord, and Ans, Elsevier, 2014, pp. 312–39. DOI.org (Crossref), doi:10.1016/B978-0-323-07954-9.00008-6
Factors that Influence SI Joint Movements

Mobility of the SI joints increases during pregnancy.
Several components, including age, sex, and the mechanical loads that are placed on the sacroiliac joint affect its movements. For example:
- The need for more mobility may be most necessary in the sacroiliac joints of younger individuals, women (around the time of pregnancy and childbirth), and athletes.4Cramer, Gregory D., and Chae-Song Ro. "The Sacrum, Sacroiliac Joint, and Coccyx." Clinical Anatomy of the Spine, Spinal Cord, and Ans, Elsevier, 2014, pp. 312–39. DOI.org (Crossref), doi:10.1016/B978-0-323-07954-9.00008-6
- The need for more stability may be most necessary in older persons, individuals who are overweight, and those who frequently carry heavy weights.4Cramer, Gregory D., and Chae-Song Ro. "The Sacrum, Sacroiliac Joint, and Coccyx." Clinical Anatomy of the Spine, Spinal Cord, and Ans, Elsevier, 2014, pp. 312–39. DOI.org (Crossref), doi:10.1016/B978-0-323-07954-9.00008-6 This increased need for stability may be accommodated by the joint’s strong ligaments and the age-associated ridges and depressions along the joint surfaces, which may promote better interlocking.3Eshed, Iris, et al. "Peripartum Changes of the Sacroiliac Joints on MRI: Increasing Mechanical Load Correlating with Signs of Edema and Inflammation Kindling Spondyloarthropathy in the Genetically Prone." Clinical Rheumatology, vol. 34, no. 8, Aug. 2015, pp. 1419–26. DOI.org (Crossref), doi:10.1007/s10067-015-2976-0
Adaptive changes in this joint also occur during pregnancy, when the joints become more mobile to compensate for the growing uterus and pelvic expansion.
Age-Related Changes in the SI Joint

Age-related changes within the SI joint can cause the lubricating fluid to deplete and joint surfaces to become inflamed.
The bones of the sacroiliac joint undergo changes as part of the natural aging process. These changes help the sacroiliac joint accommodate more forces. For example:4Cramer, Gregory D., and Chae-Song Ro. "The Sacrum, Sacroiliac Joint, and Coccyx." Clinical Anatomy of the Spine, Spinal Cord, and Ans, Elsevier, 2014, pp. 312–39. DOI.org (Crossref), doi:10.1016/B978-0-323-07954-9.00008-6
- Stability in the joint is increased. As a person approaches the end of their teenage years and begins early adulthood, the joint’s stability is primarily maintained by the ligaments. In adulthood, bony interlockings on the joint surface become enhanced to improve stability.
- Mobility in the joint is decreased. As age progresses, the movement of the sacroiliac joint reduces and is usually very minimal around the eighth decade of life.'
As the joint ages, the space between the joining bones narrows, making injection treatments, such as the sacroiliac joint injection, more challenging.7Waldman, Steven D. "Injection of the Sacroiliac Joint." Pain Management, Elsevier, 2007, pp. 1358–61. DOI.org (Crossref), doi:10.1016/B978-0-7216-0334-6.50166-7
If the joint moves more or less than usual due to an underlying problem and causes symptoms, it may indicate a medical condition called sacroiliac joint dysfunction.
See Sacroiliac Joint Dysfunction Symptoms and Causes
Osteophytes (bone spurs) and ankylosis may develop in the joints around the fourth decade of life to increase stability.4Cramer, Gregory D., and Chae-Song Ro. "The Sacrum, Sacroiliac Joint, and Coccyx." Clinical Anatomy of the Spine, Spinal Cord, and Ans, Elsevier, 2014, pp. 312–39. DOI.org (Crossref), doi:10.1016/B978-0-323-07954-9.00008-6
Variations of the Sacroiliac Joint: Implications for Pain and Discomfort
Anatomical variations of the sacroiliac joint exist in 3% to 50% of the general population. These variants may include changes to the cartilage or ligament tissues or be associated with structural changes in the adjacent bone, and typically include8Kim, Dong Kun, and Gavin A. McKenzie. "Accessory Sacroiliac Joint Injection for Relief of Buttock Pain." Pain Medicine, vol. 20, no. 2, Feb. 2019, pp. 412–13. DOI.org (Crossref), doi:10.1093/pm/pny254,9El Rafei, Mazen, et al. "Sacroiliac Joints: Anatomical Variations on MR Images." European Radiology, vol. 28, no. 12, Dec. 2018, pp. 5328–37. DOI.org (Crossref), doi:10.1007/s00330-018-5540-x:
- Accessory sacroiliac joint
- Iliosacral complex
- Bipartite iliac bony plate
- Crescent-like bony plate
The accessory sacroiliac joint is generally prone to degenerative changes and the most common symptomatic variant.
Due to its constant role in weight-bearing and unique anatomy, the sacroiliac joint(s) can become a source of pain. Symptoms can develop within the joint if the cartilage or bone gets damaged and/or when the ligaments that support the joint are strained. The vast network of nerves around the joint is highly sensitive and can transmit painful signals originating in this region.
- 1 Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. doi:10.1111/j.1469-7580.2012.01564.x
- 2 Wong M, Sinkler MA, Kiel J. Anatomy, Abdomen and Pelvis, Sacroiliac Joint. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507801/
- 4 Cramer, Gregory D., and Chae-Song Ro. "The Sacrum, Sacroiliac Joint, and Coccyx." Clinical Anatomy of the Spine, Spinal Cord, and Ans, Elsevier, 2014, pp. 312–39. DOI.org (Crossref), doi:10.1016/B978-0-323-07954-9.00008-6
- 3 Eshed, Iris, et al. "Peripartum Changes of the Sacroiliac Joints on MRI: Increasing Mechanical Load Correlating with Signs of Edema and Inflammation Kindling Spondyloarthropathy in the Genetically Prone." Clinical Rheumatology, vol. 34, no. 8, Aug. 2015, pp. 1419–26. DOI.org (Crossref), doi:10.1007/s10067-015-2976-0
- 5 Yoo WG. Effects of individual strengthening exercises for the stabilization muscles on the nutation torque of the sacroiliac joint in a sedentary worker with nonspecific sacroiliac joint pain. J Phys Ther Sci. 2015;27(1):313-314. doi:10.1589/jpts.27.313
- 6 Ombregt, Ludwig. "Disorders of the Sacroiliac Joint." A System of Orthopaedic Medicine, Elsevier, 2013, pp. 603-610.e2. DOI.org (Crossref), doi:10.1016/B978-0-7020-3145-8.00043-0
- 7 Waldman, Steven D. "Injection of the Sacroiliac Joint." Pain Management, Elsevier, 2007, pp. 1358–61. DOI.org (Crossref), doi:10.1016/B978-0-7216-0334-6.50166-7
- 8 Kim, Dong Kun, and Gavin A. McKenzie. "Accessory Sacroiliac Joint Injection for Relief of Buttock Pain." Pain Medicine, vol. 20, no. 2, Feb. 2019, pp. 412–13. DOI.org (Crossref), doi:10.1093/pm/pny254
- 9 El Rafei, Mazen, et al. "Sacroiliac Joints: Anatomical Variations on MR Images." European Radiology, vol. 28, no. 12, Dec. 2018, pp. 5328–37. DOI.org (Crossref), doi:10.1007/s00330-018-5540-x

