Sciatica is the symptom of an underlying medical condition.1Cook CE, Taylor J, Wright A, Milosavljevic S, Goode A, Whitford M. Risk Factors for First Time Incidence Sciatica: A Systematic Review. Physiotherapy Research International. 2013;19(2):65-78. doi:10.1002/pri.1572. Understanding the possible causes of sciatica can help focus treatment on addressing the root problem rather than just masking the symptoms.
The mechanism of sciatic nerve injury is either a result of direct nerve compression, inflammation, an abnormal immune system response of the body, or a combination of all these factors.2Stafford MA, Peng P, Hill DA. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. British Journal of Anaesthesia. 2007;99(4):461-473. doi:10.1093/bja/aem238.,3Kumar, M. Epidemiology, pathophysiology and symptomatic treatment of sciatica: A review. nt. J. Pharm. Bio. Arch. 2011, 2.
In This Article:
Common Causes of Sciatica
Common causes of sciatica are discussed below.
Lumbar herniated disc
Research suggests that up to 90% of sciatica is caused by a lumbar herniated disc.3Kumar, M. Epidemiology, pathophysiology and symptomatic treatment of sciatica: A review. nt. J. Pharm. Bio. Arch. 2011, 2. The herniated disc typically compresses one or more spinal nerve roots (L4-S3) that form the sciatic nerve.
A lumbar herniated disc can cause sciatica in two ways:
- Direct compression. Direct compression of the sciatic nerve can occur when a lumbar disc bulges (contained-disc-disorder) or when the soft inner material of the disc leaks out or herniates through the fibrous outer core (non-contained disc disorder) and presses against the nerve.
- Chemical inflammation. An acidic chemical irritant from the disc material (hyaluronan) may leak out and cause inflammation and irritation in the area around the sciatic nerve.3Kumar, M. Epidemiology, pathophysiology and symptomatic treatment of sciatica: A review. nt. J. Pharm. Bio. Arch. 2011, 2.,4Gore S, Nadkarni S. Sciatica: detection and confirmation by new method. Int J Spine Surg. 2014;8:15. Published 2014 Dec 1. doi:10.14444/1015.,5Molinos M, Almeida CR, Caldeira J, Cunha C, Gonçalves RM, Barbosa MA. Inflammation in intervertebral disc degeneration and regeneration [published correction appears in J R Soc Interface. 2015 Jul 6;12(108):20150429]. J R Soc Interface. 2015;12(104):20141191. doi:10.1098/rsif.2014.1191.
A herniated disc may compress the sciatic nerve on one side, causing symptoms in one leg, or the disc may bulge or herniate from both sides, causing symptoms in both legs (bilateral sciatica). Bilateral sciatica may also be caused by two adjacent segment discs herniating on either side, although this possibility is rare.
Degeneration
Degeneration of tissues in the lumbar spine can compress or irritate the sciatic nerve roots in several ways:
- Degeneration of the facet joints can cause the synovial tissue in the joint’s capsule to inflame and increase in bulk.
- Degeneration of vertebral bone may cause abnormal bone growths (bone spurs or osteophytes). These abnormally bulky tissues in the lumbar spine may cause compression of one or more nerve roots of the sciatic nerve.
Degenerated intervertebral discs may secrete inflammatory proteins, causing inflammation of the sciatic nerve.6Donnally III CJ, Varacallo M. Lumbar Degenerative Disk Disease. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448134/.,7Valat J-P, Genevay S, Marty M, Rozenberg S, Koes B. Sciatica. Best Practice & Research Clinical Rheumatology. 2010;24(2):241-252. doi:10.1016/j.berh.2009.11.005.
Depending on the severity, the nerve roots may cause varying symptoms in the low back and leg.
Lumbar spinal stenosis
Lumbar spinal stenosis is the narrowing of the spinal canal and is relatively common in adults older than age 60.8Melancia JL, Francisco AF, Antunes JL. Spinal stenosis. In: Handbook of Clinical Neurology. Elsevier; 2014:541-549. doi:10.1016/b978-0-7020-4086-3.00035-7. Research suggests that lateral recess stenosis may be common in causing sciatica in the elderly population.9Ombregt L. The dural concept. In: A System of Orthopaedic Medicine. Elsevier; 2013:447-472.e4. doi:10.1016/b978-0-7020-3145-8.00033-8.
Watch: Lumbar Spinal Stenosis Video
Spondylolisthesis
Spondylolisthesis occurs when a small stress fracture causes one vertebral body to slip forward on another.
For example, the L5 vertebra may slip forward over the S1 vertebra. Sciatica may result from nerve compression following the disc space collapse, fracture, and forward slipping of the vertebral body. Spondylolisthesis may cause bilateral sciatica and is more common in younger adults.9Ombregt L. The dural concept. In: A System of Orthopaedic Medicine. Elsevier; 2013:447-472.e4. doi:10.1016/b978-0-7020-3145-8.00033-8.
Watch: Isthmic Spondylolisthesis Video
These conditions may develop over time or spontaneously due to trauma or physical stress injury. Motor vehicle accidents, sports injuries, or falls may cause direct injury to the sciatic nerve. Conditions such as spondylolisthesis and herniated discs may develop from physical stress injuries, such as from weightlifting.
Lower Back Conditions that Cause Sciatica-Like Symptoms
Some lower back conditions may cause sciatica-like symptoms. A few examples are discussed below.
Piriformis syndrome

The symptoms of piriformis syndrome may mimic sciatica.
Piriformis syndrome is caused by spasms of the piriformis muscle. Sciatica symptoms may occur when the inflamed muscle irritates or compresses the sciatic nerve at its origin.
Piriformis syndrome is more common when the sciatic nerve is split, which is a normal variant near the piriformis muscle, or in normal anatomical variations of the piriformis muscles itself.10Eastlack J, Tenorio L, Wadhwa V, Scott K, Starr A, Chhabra A. Sciatic neuromuscular variants on MR neurography: frequency study and interobserver performance. Br J Radiol. 2017;90(1079):20170116. doi:10.1259/bjr.20170116. Piriformis syndrome is also common in overuse injuries, particularly in runners and athletes.11Davis D, Vasudevan A. Sciatica. [Updated 2019 Feb 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/.
Watch: Piriformis Syndrome Video
Sacroiliac joint dysfunction
Irritation of the sacroiliac joint—located at the bottom of the spine—can also irritate the L5 nerve, which lies on top of the sacroiliac joint, causing sciatica-type pain.
See Sacroiliac Joint Dysfunction (SI Joint Pain)
In these cases, there is no true radiculopathy or radiating nerve pain. However, the resulting leg pain typically feels like sciatica.
Less Common Causes of Sciatica

Spinal tumors may sometimes cause sciatica symptoms.
Rarely, sciatica may develop due to tumors, infection, formation of scar tissue, collection of fluid, Pott’s disease (spinal tuberculosis), or fracture in the lumbar spine. While rare, sciatica may also develop as a complication of incorrect muscular injection methods in the buttock or following a hip joint replacement surgery.12Gujrathi R, Gupta K, Ravi C, Pai B. Sciatica: An Extremely Rare Complication of the Perianal Abscess. Pol J Radiol. 2016;81:370–373. Published 2016 Aug 6. doi:10.12659/PJR.897269. Approximately 1% of pregnant women may develop sciatica at some point during pregnancy.13Katonis P, Kampouroglou A, Aggelopoulos A, et al. Pregnancy-related low back pain. Hippokratia. 2011;15(3):205–210.
Risk Factors for Sciatica
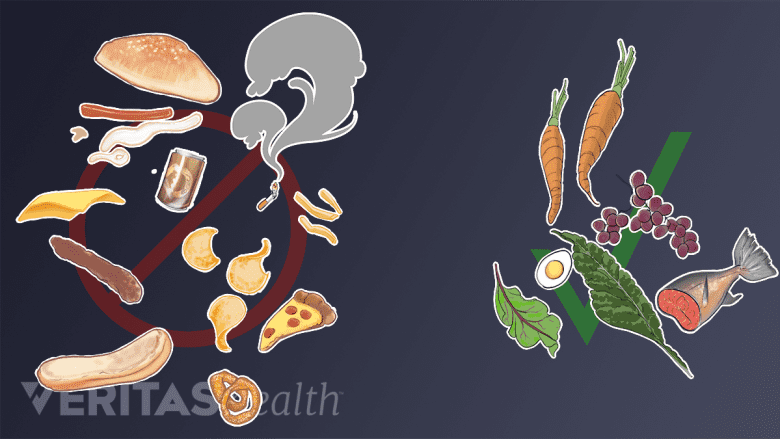
Smoking and following unhealthy eating habits can increase the risk of sciatica.
The presence of certain risk factors may increase the likelihood of developing sciatica. A few examples include:
- Smoking
- Mental health issues, such as depression
- Tall height in older age groups (50 to 60 years)
- Obesity and excess weight
- Genetic susceptibility
- Vitamin B 12 deficiency
- Physical deconditioning from a sedentary, inactive lifestyle
- Certain types of occupation (such as truck drivers, carpenters, or machine operators)
- Poor work ergonomics
The presence of these risk factors alone does not establish the cause for sciatica development. However, these factors combined with an individual’s age and general health may play a role in causing sciatica to develop.
It is advisable to see a doctor if sciatica symptoms are experienced. Sciatica typically improves considerably if treated early and may become chronic or more severe if left untreated for a long time.
Watch Sciatica Treatment Video
- 1 Cook CE, Taylor J, Wright A, Milosavljevic S, Goode A, Whitford M. Risk Factors for First Time Incidence Sciatica: A Systematic Review. Physiotherapy Research International. 2013;19(2):65-78. doi:10.1002/pri.1572.
- 2 Stafford MA, Peng P, Hill DA. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. British Journal of Anaesthesia. 2007;99(4):461-473. doi:10.1093/bja/aem238.
- 3 Kumar, M. Epidemiology, pathophysiology and symptomatic treatment of sciatica: A review. nt. J. Pharm. Bio. Arch. 2011, 2.
- 4 Gore S, Nadkarni S. Sciatica: detection and confirmation by new method. Int J Spine Surg. 2014;8:15. Published 2014 Dec 1. doi:10.14444/1015.
- 5 Molinos M, Almeida CR, Caldeira J, Cunha C, Gonçalves RM, Barbosa MA. Inflammation in intervertebral disc degeneration and regeneration [published correction appears in J R Soc Interface. 2015 Jul 6;12(108):20150429]. J R Soc Interface. 2015;12(104):20141191. doi:10.1098/rsif.2014.1191.
- 6 Donnally III CJ, Varacallo M. Lumbar Degenerative Disk Disease. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448134/.
- 7 Valat J-P, Genevay S, Marty M, Rozenberg S, Koes B. Sciatica. Best Practice & Research Clinical Rheumatology. 2010;24(2):241-252. doi:10.1016/j.berh.2009.11.005.
- 8 Melancia JL, Francisco AF, Antunes JL. Spinal stenosis. In: Handbook of Clinical Neurology. Elsevier; 2014:541-549. doi:10.1016/b978-0-7020-4086-3.00035-7.
- 9 Ombregt L. The dural concept. In: A System of Orthopaedic Medicine. Elsevier; 2013:447-472.e4. doi:10.1016/b978-0-7020-3145-8.00033-8.
- 10 Eastlack J, Tenorio L, Wadhwa V, Scott K, Starr A, Chhabra A. Sciatic neuromuscular variants on MR neurography: frequency study and interobserver performance. Br J Radiol. 2017;90(1079):20170116. doi:10.1259/bjr.20170116.
- 11 Davis D, Vasudevan A. Sciatica. [Updated 2019 Feb 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/.
- 12 Gujrathi R, Gupta K, Ravi C, Pai B. Sciatica: An Extremely Rare Complication of the Perianal Abscess. Pol J Radiol. 2016;81:370–373. Published 2016 Aug 6. doi:10.12659/PJR.897269.
- 13 Katonis P, Kampouroglou A, Aggelopoulos A, et al. Pregnancy-related low back pain. Hippokratia. 2011;15(3):205–210.

