When a surgeon and patient decide to move ahead with spine surgery for low back pain, it is crucial that they have clear and detailed conversations about the type and purpose of the surgery, including the risks, healing process, recovery time, return to activities and activity restrictions, and the potential outcomes of the surgery—so that they can have similar expectations and goals.
For example, spinal fusion surgery is typically more complex than a microdiscectomy.
The outcome of surgery depends on the duration of symptoms, type of condition being treated, nature of the surgery, general health and mental well-being of the patient, and skill of the surgeon.
In This Article:
- Lumbar Spine Surgery
- Types of Lumbar Spine Surgeries: What You Need to Know
- What to Expect from Spine Surgery for Low Back Pain
- Lumbar Spine Surgery Alternatives
- Video: Am I a Candidate for Back Surgery?
Spine Surgery for Treating Back Pain and Leg Pain (Sciatica)
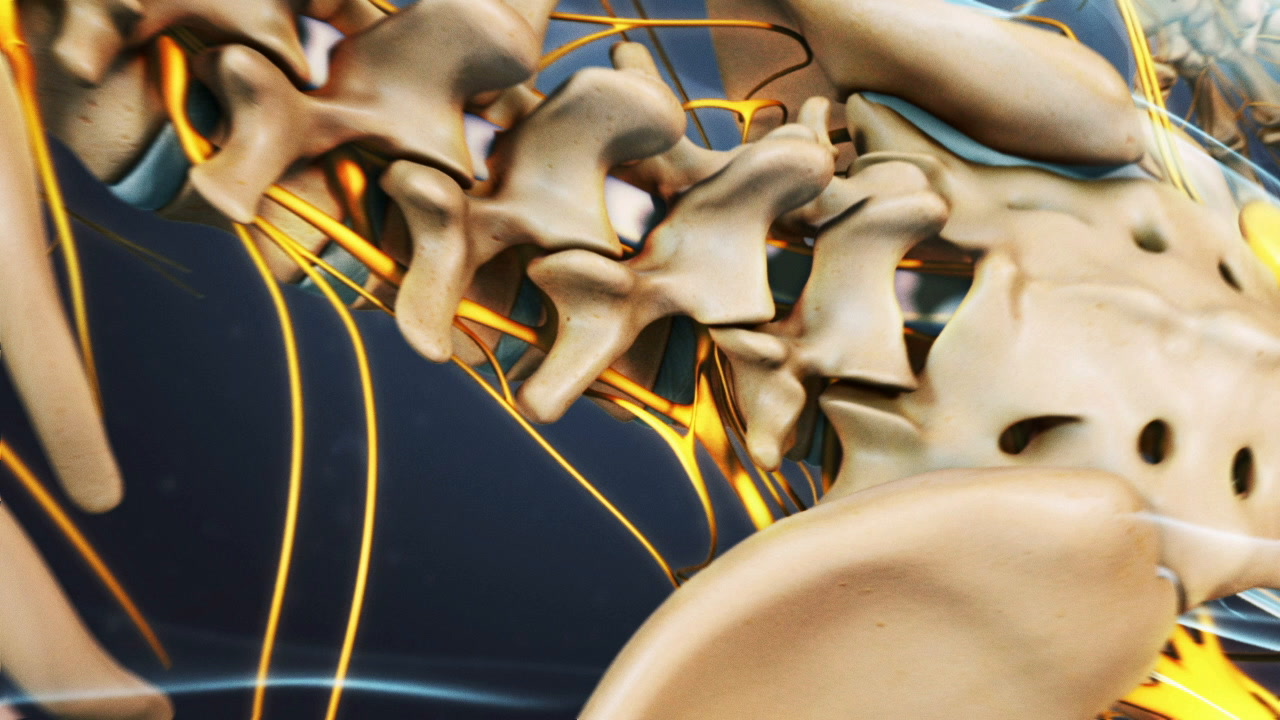
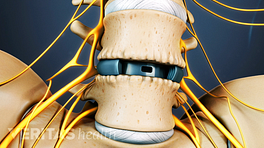
Leg pain and back pain from a pinched nerve in the lower spine, commonly called sciatica and medically known as lumbar radiculopathy, mainly occurs due to a lumbar herniated disc. A common surgical treatment for herniated discs is a decompression surgery called lumbar discectomy.
What is the success rate?
Lumbar discectomy typically yields a high success rate, with over 79% of patients experiencing satisfactory, good, or excellent results from their surgery over a period of 6 years post-surgery. 1 Dohrmann GJ, Mansour N. Long-Term Results of Various Operations for Lumbar Disc Herniation: Analysis of over 39,000 Patients. Med Princ Pract. 2015;24(3):285-290. doi:10.1159/000375499 The surgery is primarily done via minimally invasive procedures and involves faster healing and recovery.
How fast do the symptoms resolve?
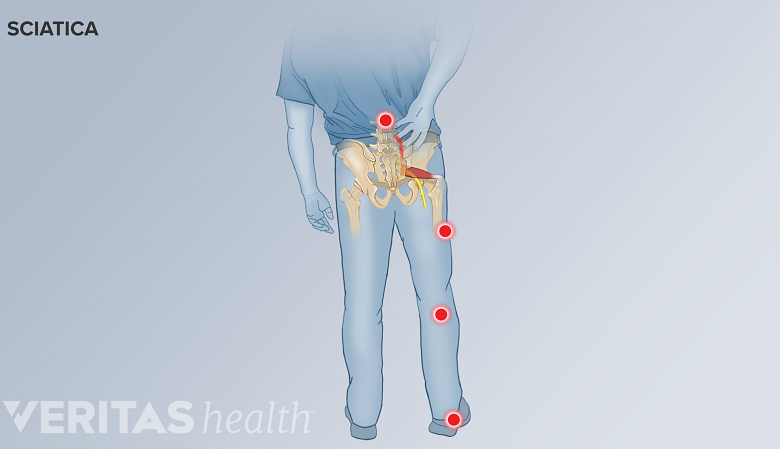
Areas of pain distribution in sciatica.
The main symptoms of sciatica are leg pain, paresthesia (abnormal sensations like pins and needles), and numbness.
A study evaluating the resolution of these symptoms after surgical decompression in 85 patients found that 2 Huang P, Sengupta DK. How fast pain, numbness, and paresthesia resolves after lumbar nerve root decompression: a retrospective study of patientʼs self-reported computerized pain drawing. Spine. 2014;39(8):E529-E536. doi:10.1097/BRS.0000000000000240 :
- Pain recovers first, with maximum improvement occurring during the initial 6 weeks, and plateauing at 3 months.
- Paresthesia improves in the first 3 months and no further improvements are typically seen after the 3-month mark.
- Numbness improves at a slower pace and the recovery continues through the first year after surgery.
It was noted that patients who had symptoms for 6 months or less before surgery experienced faster recovery than patients who had pre-surgical symptoms for more than 6 months. 2 Huang P, Sengupta DK. How fast pain, numbness, and paresthesia resolves after lumbar nerve root decompression: a retrospective study of patientʼs self-reported computerized pain drawing. Spine. 2014;39(8):E529-E536. doi:10.1097/BRS.0000000000000240
Spine Surgery for Treating Back Pain
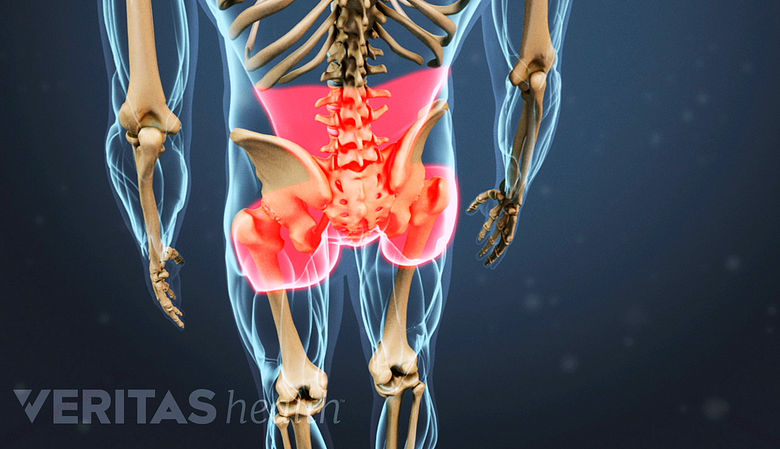
Axial back pain is typically confined to the lower back area.
Localized back pain, also called axial back pain, without leg pain is more challenging to treat compared to sciatica.
Surgery is generally not indicated for axial back pain, but select patients with severe back pain may be treated with smaller decompression procedures if a specific pathology is identified in the spine and suspected to be the cause of back pain. 3 Macki M, Hamilton T, Massie L, et al. Characteristics and outcomes of patients undergoing lumbar spine surgery for axial back pain in the Michigan Spine Surgery Improvement Collaborative. Spine J. 2022;22(10):1651-1659. doi:10.1016/j.spinee.2022.06.013
Factors that affect the long-term outlook
A study involving around 300 patients who underwent spinal decompression surgery for axial back pain found that 3 Macki M, Hamilton T, Massie L, et al. Characteristics and outcomes of patients undergoing lumbar spine surgery for axial back pain in the Michigan Spine Surgery Improvement Collaborative. Spine J. 2022;22(10):1651-1659. doi:10.1016/j.spinee.2022.06.013 :
- 90 days after the surgery: Patients with multilevel surgery had more pain compared to patients with single-level surgeries.
- 1 year after the surgery: Patients who had pre-surgical pain symptoms for more than a year were 16% more likely to experience post-surgical pain compared to their counterparts who decided on surgery sooner.
- 2 years after surgery: Patients who had depression were 30% more likely to experience post-surgical pain.
Limited research supports high-frequency spinal cord stimulation (SCS) for treating axial back pain but more studies are needed to establish the efficacy of this treatment. 4 Al-Kaisy A, Palmisani S, Smith TE, et al. Long-Term Improvements in Chronic Axial Low Back Pain Patients Without Previous Spinal Surgery: A Cohort Analysis of 10-kHz High-Frequency Spinal Cord Stimulation over 36 Months. Pain Med. 2018;19(6):1219-1226. doi:10.1093/pm/pnx237 , 5 Conger A, Sperry BP, Cheney CW, et al. The Effectiveness of Spinal Cord Stimulation for the Treatment of Axial Low Back Pain: A Systematic Review with Narrative Synthesis. Pain Med. 2020;21(11):2699-2712. doi:10.1093/pm/pnaa142
Recovery from spinal surgery largely depends on the extent and type of surgery, the number of levels that were treated, the patient’s age and concomitant medical conditions, and how closely the care instructions are followed.
If the recovery and outcome of a surgery is not as expected, it is important to communicate the concerns with the surgeon. Failed back surgery can be treated through several non-surgical treatments and sometimes through revision surgery based on the cause of pain.
- 1 Dohrmann GJ, Mansour N. Long-Term Results of Various Operations for Lumbar Disc Herniation: Analysis of over 39,000 Patients. Med Princ Pract. 2015;24(3):285-290. doi:10.1159/000375499
- 2 Huang P, Sengupta DK. How fast pain, numbness, and paresthesia resolves after lumbar nerve root decompression: a retrospective study of patientʼs self-reported computerized pain drawing. Spine. 2014;39(8):E529-E536. doi:10.1097/BRS.0000000000000240
- 3 Macki M, Hamilton T, Massie L, et al. Characteristics and outcomes of patients undergoing lumbar spine surgery for axial back pain in the Michigan Spine Surgery Improvement Collaborative. Spine J. 2022;22(10):1651-1659. doi:10.1016/j.spinee.2022.06.013
- 4 Al-Kaisy A, Palmisani S, Smith TE, et al. Long-Term Improvements in Chronic Axial Low Back Pain Patients Without Previous Spinal Surgery: A Cohort Analysis of 10-kHz High-Frequency Spinal Cord Stimulation over 36 Months. Pain Med. 2018;19(6):1219-1226. doi:10.1093/pm/pnx237
- 5 Conger A, Sperry BP, Cheney CW, et al. The Effectiveness of Spinal Cord Stimulation for the Treatment of Axial Low Back Pain: A Systematic Review with Narrative Synthesis. Pain Med. 2020;21(11):2699-2712. doi:10.1093/pm/pnaa142