As with any injection procedure, potential side effects and risks are possible with lumbar epidural steroid injections. The side effects are usually temporary and tolerable. Rarely, serious adverse events may occur.1Pountos I, Panteli M, Walters G, Bush D, Giannoudis PV. Safety of Epidural Corticosteroid Injections. Drugs R D. 2016;16(1):19–34. doi:10.1007/s40268-015-0119-3
The most common risk is that the injection does not provide any, or only provides minimal, pain relief. It is disappointing to go through the procedure and not experience a meaningful reduction in pain, or to find that the initial pain relief is fleeting, and the original pain returns after a few weeks.
Possible Side Effects of Epidural Steroid Injections
Headache is a common side effect of epidural steroid injection.
Side effects after an epidural are usually not serious. A few examples include (but are not limited to)2Manchikanti L, Buenaventura RM, Manchikanti KN, et al. Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Physician. 2012;15(3):E199-245. Available from: https://pubmed.ncbi.nlm.nih.gov/22622912/,3Ter Meulen BC, Maas ET, Vyas A, et al. Treatment of acute sciatica with transforaminal epidural corticosteroids and local anesthetic: design of a randomized controlled trial. BMC Musculoskelet Disord. 2017;18(1):215. Published 2017 May 25. doi:10.1186/s12891-017-1571-8:
- Nausea
- Headache
- Dizziness
- Fainting due to anxiety from the procedure causing a sudden decrease in heart rate and blood pressure (vasovagal attack)
- Flushing of the face (redness and a feeling of warmth)
In This Article:
- Lumbar Epidural Steroid Injections for Low Back Pain and Sciatica
- How Epidural Steroid Injections Work
- Indications for Lumbar Epidural Injections
- Epidural Injection Procedure
- Epidural Steroid Injection Pain Relief Success Rates
- Epidural Steroid Injections: Risks and Side Effects
- Epidural Steroid Injections for Back Pain and Leg Pain Video
These side effects typically resolve with rest. Injection site pain, if present, may be treated with cold therapy using ice packs to reduce pain and/or swelling.
Potential Complications and Adverse Events after an Epidural Steroid Injection
While rare, serious complications are possible after an epidural steroid injection and are discussed below.
Infection

Meningitis is a potential adverse event associated with epidural steroid injections.
Infections may occur generally within the body (systemic infection), affect the brain and/or spinal cord, or occur locally in the area of the injection. Examples include4Manchikanti L, Kaye AD, Falco FJE, Hirsch JA. Essentials of Interventional Techniques in Managing Chronic Pain. Cham, Switzerland: Springer; 2018.:
- Epidural abscess: Accumulation of pus in the epidural space.
- Meningitis: Inflammation of the brain and spinal cord membranes.
- Osteomyelitis or discitis: Infection of the vertebral bone or disc.
- Soft tissue abscess: Accumulation of pus within the soft tissues at the site of injection.
Microbes from the patient’s skin are believed to be a common cause of infections.1Pountos I, Panteli M, Walters G, Bush D, Giannoudis PV. Safety of Epidural Corticosteroid Injections. Drugs R D. 2016;16(1):19–34. doi:10.1007/s40268-015-0119-3
Bleeding
Damage to arteries may cause localized bleeding and pooling of blood within the soft tissues, epidural space, or membranes of the spinal cord. A hematoma or blood clot may form within the artery, blocking the blood supply to vital tissues, such as the brain and/or spinal cord.4Manchikanti L, Kaye AD, Falco FJE, Hirsch JA. Essentials of Interventional Techniques in Managing Chronic Pain. Cham, Switzerland: Springer; 2018.
Dural puncture
Inadvertently inserting the needle into the spinal cord’s outer membrane (dura mater) may cause a dural puncture.4Manchikanti L, Kaye AD, Falco FJE, Hirsch JA. Essentials of Interventional Techniques in Managing Chronic Pain. Cham, Switzerland: Springer; 2018. This condition is also called a wet tap and causes the cerebrospinal fluid (CSF) to leak out, decreasing CSF pressure in the brain, resulting in a headache.
Nerve damage
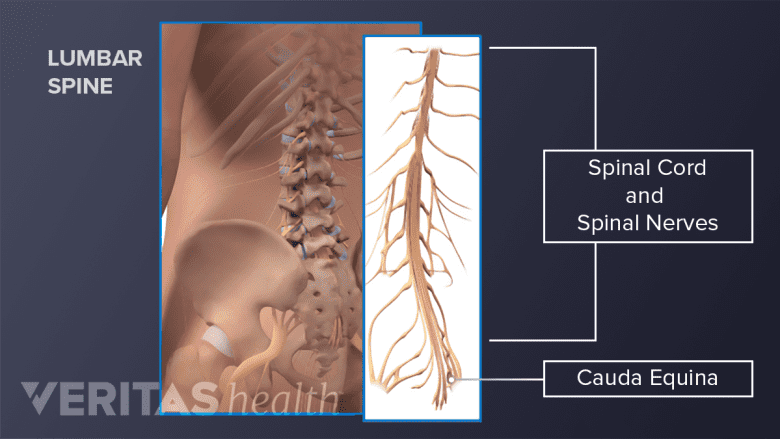
Damage to the cauda equina nerves is a medical emergency.
Damage to neighboring nerves may cause abnormal sensations, loss of sensation, or seizures. If the cauda equina nerves are damaged at the base of the spinal cord, it may result in a medical emergency called cauda equina syndrome. This syndrome causes loss of bowel and bladder control and must be treated immediately to prevent paralysis of the lower body.4Manchikanti L, Kaye AD, Falco FJE, Hirsch JA. Essentials of Interventional Techniques in Managing Chronic Pain. Cham, Switzerland: Springer; 2018.
Cardiovascular system (heart) complications
Sometimes, low blood pressure and decreased heart rate may occur after an epidural steroid injection.4Manchikanti L, Kaye AD, Falco FJE, Hirsch JA. Essentials of Interventional Techniques in Managing Chronic Pain. Cham, Switzerland: Springer; 2018.
Risk associated with local anesthetics
In injections containing local anesthetics, if the solution enters a blood vessel, it may result in toxicity of the central nervous system and/or the cardiovascular system.5Chang, Douglas, Zlomislic, Vinko. Chapter 273. Lumbar Spinal Injections. In: Chapman, Michael W. Chapman's Orthopaedic Surgery. Philadelphia: Lippincott Williams & Wilkins. https://www.researchgate.net/publication/327034223_Lumbar_spinal_injections_Chapman's_Orthopaedic_Surgery_Chapter_273. Accessed June 26, 2019.
Risk associated with particulate steroids
Larger particles in particulate steroids may lump together and block blood vessels, causing reduced blood supply to the spinal cord.5Chang, Douglas, Zlomislic, Vinko. Chapter 273. Lumbar Spinal Injections. In: Chapman, Michael W. Chapman's Orthopaedic Surgery. Philadelphia: Lippincott Williams & Wilkins. https://www.researchgate.net/publication/327034223_Lumbar_spinal_injections_Chapman's_Orthopaedic_Surgery_Chapter_273. Accessed June 26, 2019.,6Hassan KZ, Sherman Al. Epidural Steroids. [Updated 2019 May 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK537320/,7Dietrich TJ, Sutter R, Froehlich JM, Pfirrmann CWA. Particulate versus non-particulate steroids for lumbar transforaminal or interlaminar epidural steroid injections: an update. Skeletal Radiology. 2014;44(2):149-155. doi:10.1007/s00256-014-2048-6
Risks and complications are typically higher in epidural steroid injections administered above the L3 level.3Ter Meulen BC, Maas ET, Vyas A, et al. Treatment of acute sciatica with transforaminal epidural corticosteroids and local anesthetic: design of a randomized controlled trial. BMC Musculoskelet Disord. 2017;18(1):215. Published 2017 May 25. doi:10.1186/s12891-017-1571-8,8Schneider B, Varghis N, Kennedy DJ. Ideal Corticosteroid Choice for Epidural Steroid Injections: A Review of Safety and Efficacy. Curr Phys Med Rehabil Rep (2015) 3:151–158 DOI 10.1007/s40141-015-0086-1 The most common risk is the injection of steroids into a blood vessel, which becomes more likely to occur in people over 50 years of age.7Dietrich TJ, Sutter R, Froehlich JM, Pfirrmann CWA. Particulate versus non-particulate steroids for lumbar transforaminal or interlaminar epidural steroid injections: an update. Skeletal Radiology. 2014;44(2):149-155. doi:10.1007/s00256-014-2048-6 Rarely, an allergic reaction to the steroids, local anesthetic, or contrast dye may occur.
When to Seek Immediate Medical Attention: Red Flag Symptoms and Signs
Serious symptoms following an epidural steroid injection that require immediate medical attention include:
- Severe headache while sitting up or standing that feels better after lying down, which may indicate a dural puncture
- A fever of 101 degrees or greater, which may indicate an infection
- Reduced or complete loss of bowel or bladder control while the patient is still numb or after the local anesthetic and temporary numbness wear off, which may indicate medical emergencies, such as cauda equina syndrome
- A feeling of numbness and/or weakness in the leg(s), which may indicate nerve injury
It is important to call the doctor immediately if these symptoms occur. Additionally, any discomfort or abnormal feeling must be discussed with the doctor.
- 1 Pountos I, Panteli M, Walters G, Bush D, Giannoudis PV. Safety of Epidural Corticosteroid Injections. Drugs R D. 2016;16(1):19–34. doi:10.1007/s40268-015-0119-3
- 2 Manchikanti L, Buenaventura RM, Manchikanti KN, et al. Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Physician. 2012;15(3):E199-245. Available from: https://pubmed.ncbi.nlm.nih.gov/22622912/
- 3 Ter Meulen BC, Maas ET, Vyas A, et al. Treatment of acute sciatica with transforaminal epidural corticosteroids and local anesthetic: design of a randomized controlled trial. BMC Musculoskelet Disord. 2017;18(1):215. Published 2017 May 25. doi:10.1186/s12891-017-1571-8
- 4 Manchikanti L, Kaye AD, Falco FJE, Hirsch JA. Essentials of Interventional Techniques in Managing Chronic Pain. Cham, Switzerland: Springer; 2018.
- 5 Chang, Douglas, Zlomislic, Vinko. Chapter 273. Lumbar Spinal Injections. In: Chapman, Michael W. Chapman's Orthopaedic Surgery. Philadelphia: Lippincott Williams & Wilkins. https://www.researchgate.net/publication/327034223_Lumbar_spinal_injections_Chapman's_Orthopaedic_Surgery_Chapter_273. Accessed June 26, 2019.
- 6 Hassan KZ, Sherman Al. Epidural Steroids. [Updated 2019 May 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK537320/
- 7 Dietrich TJ, Sutter R, Froehlich JM, Pfirrmann CWA. Particulate versus non-particulate steroids for lumbar transforaminal or interlaminar epidural steroid injections: an update. Skeletal Radiology. 2014;44(2):149-155. doi:10.1007/s00256-014-2048-6
- 8 Schneider B, Varghis N, Kennedy DJ. Ideal Corticosteroid Choice for Epidural Steroid Injections: A Review of Safety and Efficacy. Curr Phys Med Rehabil Rep (2015) 3:151–158 DOI 10.1007/s40141-015-0086-1

